Childbirth Maternal Mortality Black Women
Childbirth maternal mortality black women is a deeply concerning issue in the United States, highlighting the stark racial disparities in maternal health outcomes. This blog post delves into the historical context, socioeconomic factors, and healthcare access issues contributing to this tragedy. We examine the specific risks faced by Black women, explore cultural considerations, and analyze the current data and research gaps.
Ultimately, the goal is to understand the complexities of this problem and identify potential solutions to improve maternal health for all women.
The historical legacy of systemic racism and discrimination has profoundly shaped the experiences of Black women throughout their lives, including their pregnancies and deliveries. This has resulted in significant disparities in access to quality healthcare, impacting their health outcomes. We will explore the many layers of this complex issue.
Historical Context
Maternal mortality, tragically, remains a significant public health concern, particularly for Black women in the United States. Understanding the historical context is crucial to appreciating the ongoing disparities and the need for targeted interventions. This deep-rooted issue is intertwined with systemic inequalities that have persisted for generations, shaping healthcare access, social determinants, and ultimately, maternal outcomes.The legacy of systemic racism and its impact on Black women’s health has created a complex web of factors contributing to higher maternal mortality rates.
These factors extend far beyond the immediate birthing experience and are deeply rooted in historical and ongoing injustices.
Historical Overview of Maternal Mortality Rates Among Black Women
The stark reality of higher maternal mortality among Black women in the US is not a new phenomenon. Historical data reveals a persistent and disturbing pattern, highlighting the systemic challenges that have plagued Black communities. This disparity in outcomes reflects the broader historical injustices and inequalities faced by Black Americans.
Social and Economic Factors
Throughout US history, Black women have faced significant social and economic disadvantages. These disadvantages have created barriers to accessing quality healthcare, leading to poorer maternal health outcomes. Poverty, lack of affordable housing, limited access to nutritious food, and exposure to environmental hazards are all factors that contribute to a higher risk of adverse pregnancy outcomes. Discrimination in the healthcare system, and lack of culturally competent care, further compound these challenges.
These factors have been instrumental in creating a cycle of disadvantage for Black women and their families.
Evolution of Healthcare Access and Quality for Black Women During Childbirth
The quality of healthcare received by Black women during childbirth has evolved, but disparities persist. Early forms of healthcare were often inadequate and inaccessible to Black women, often resulting in inadequate prenatal care, limited access to skilled providers, and potentially life-threatening complications. While significant advancements in medical technology and procedures have occurred, these gains have not been evenly distributed.
The legacy of implicit bias and discrimination within the healthcare system continues to impact Black women’s access to high-quality care. This ongoing struggle to overcome historical injustices is vital to address.
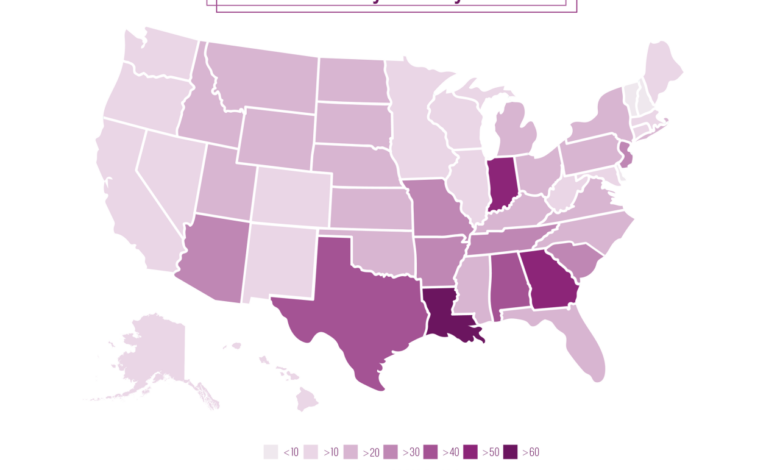
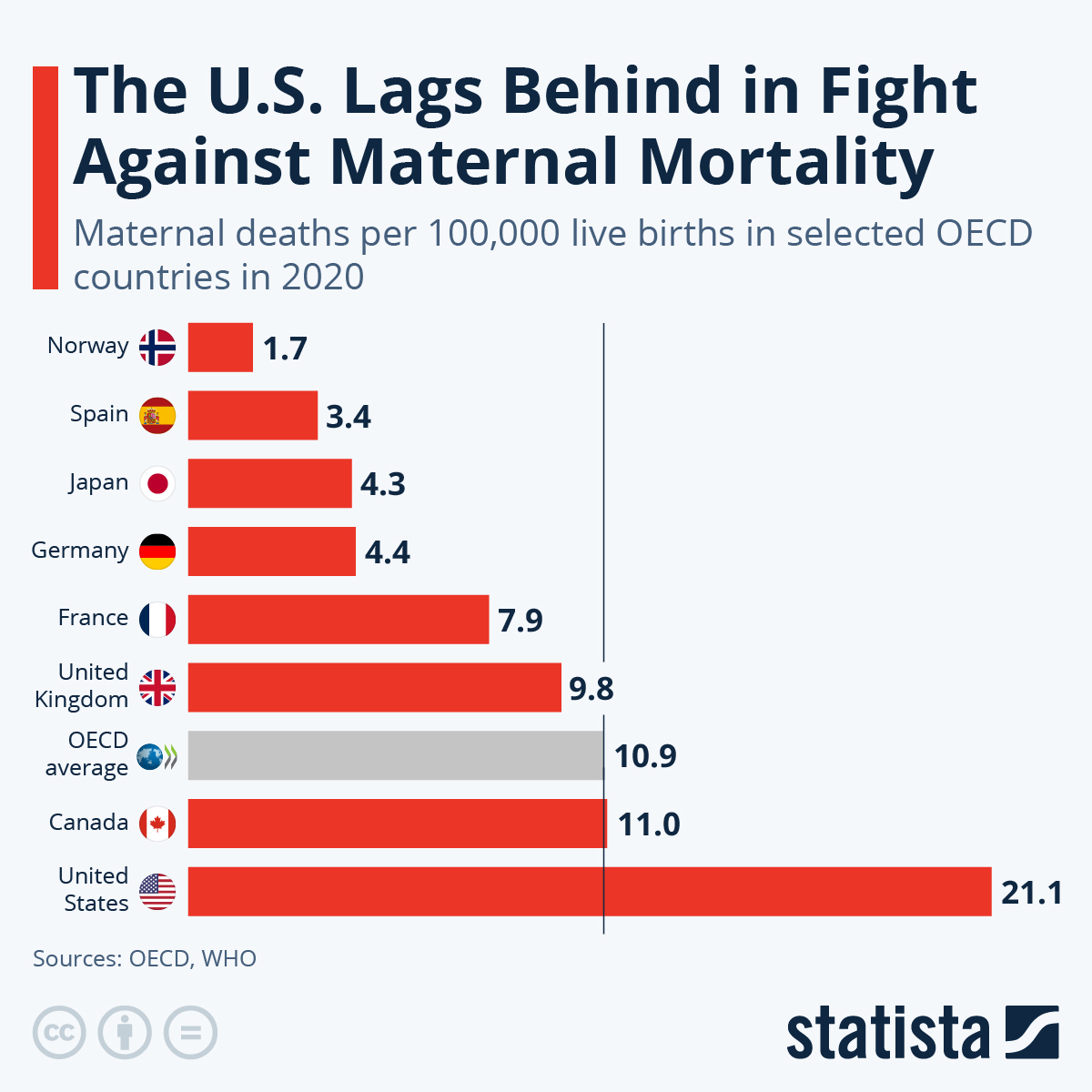
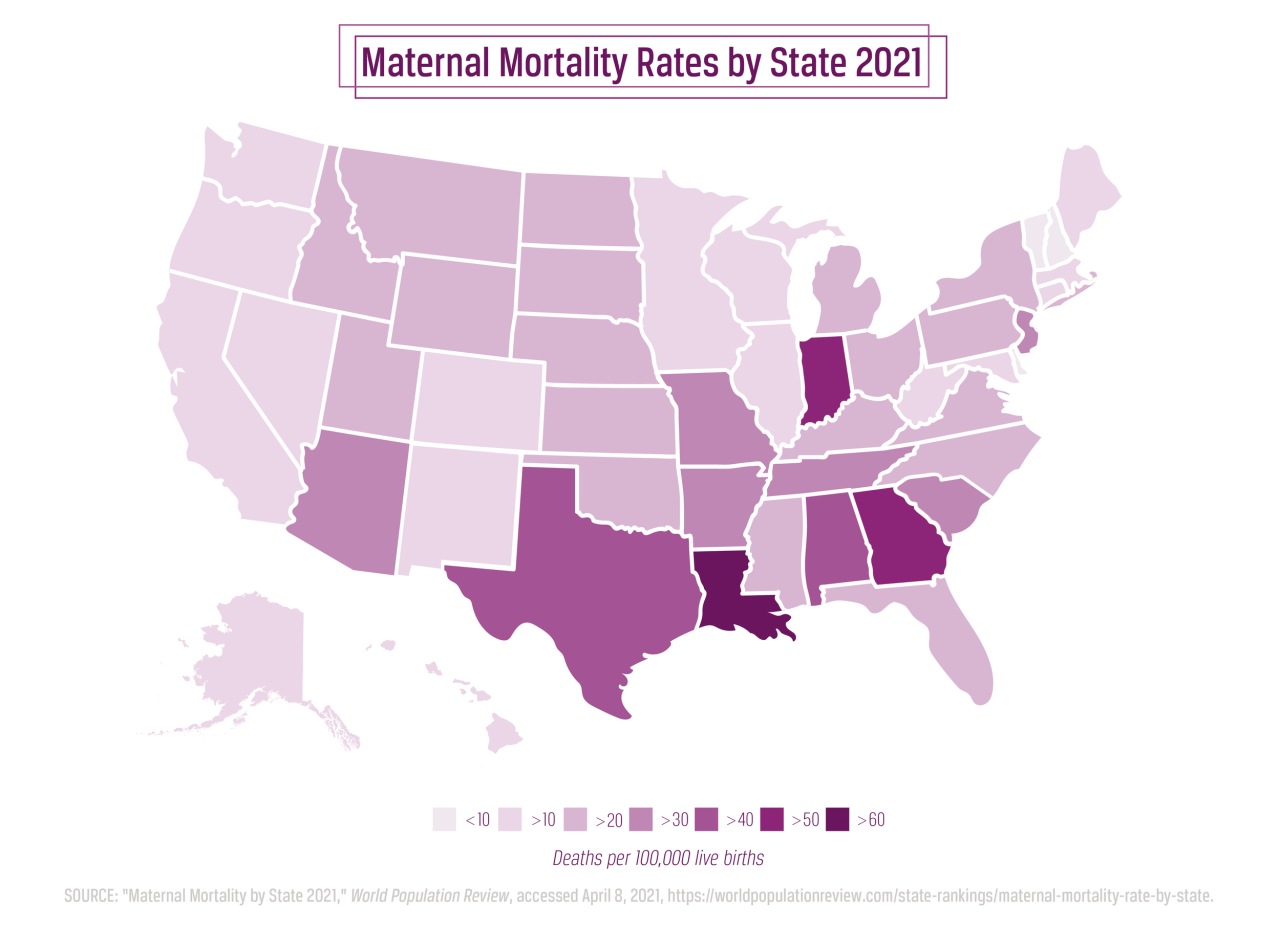
Comparison of Maternal Mortality Rates
Comparing maternal mortality rates across racial groups reveals a stark contrast. Data consistently demonstrates a higher rate of maternal mortality among Black women compared to other racial groups in the United States. This difference underscores the need for focused strategies to address the unique challenges faced by Black women during pregnancy and childbirth. The significant disparity demands that interventions specifically address these systemic issues.
Maternal Mortality Rates for Black Women
| Year | Maternal Mortality Rate (per 100,000 live births) |
|---|---|
| 2017 | 56.1 |
| 2018 | 53.6 |
| 2019 | 52.3 |
| 2020 | 57.1 |
Note: These rates are estimates based on available data and may vary depending on the source. The table showcases a complex picture, where despite some fluctuations, the persistent disparity in maternal mortality rates for Black women remains evident.
Socioeconomic Factors
The stark reality of childbirth disparities for Black women is deeply intertwined with socioeconomic factors. These factors create systemic barriers that compound the existing challenges, perpetuating cycles of disadvantage and ultimately contributing to higher maternal mortality rates. Understanding these interconnected issues is crucial to developing effective interventions and strategies to address this pressing public health concern.Poverty, limited access to quality healthcare, and restricted educational opportunities act as significant obstacles for Black women navigating the complexities of pregnancy and childbirth.
These factors, frequently intertwined and reinforcing one another, create a vicious cycle of disadvantage that is difficult to break. The consequences of these socioeconomic disparities are reflected in the disproportionate maternal mortality rates experienced by Black women.
Poverty and Healthcare Access
Poverty often limits access to essential prenatal care, including regular check-ups, necessary screenings, and adequate nutrition. Lack of access to quality healthcare translates into delayed or missed diagnoses of potential complications, increased risk of developing pregnancy-related conditions, and potentially inadequate management of existing health issues. Furthermore, individuals experiencing poverty may face challenges in affording necessary medications and treatments, exacerbating existing health vulnerabilities.
This is further complicated by the fact that many Black women experience higher rates of chronic conditions, like hypertension and diabetes, which can lead to more severe pregnancy complications if not properly managed.
Limited Educational Opportunities
Limited educational opportunities often correlate with lower earning potential and fewer economic resources. This can further restrict access to quality healthcare and create a cycle of disadvantage. Lack of education may also result in a reduced understanding of maternal health risks and preventative measures. Women with limited education may have less awareness of the importance of regular prenatal care, leading to delayed or missed appointments.
This limited understanding can also affect their ability to advocate for their own health needs within the healthcare system.
Socioeconomic Status and Maternal Mortality Rates
The correlation between socioeconomic status and maternal mortality rates is undeniable. Studies consistently show a strong association between lower socioeconomic status and a heightened risk of maternal mortality among Black women. Women with limited economic resources often face barriers to accessing adequate healthcare, nutritious food, and safe housing, all of which contribute to adverse pregnancy outcomes. For example, the lack of access to transportation to healthcare facilities can deter women from seeking necessary prenatal care.
Implicit Bias in Healthcare
Implicit bias in healthcare settings significantly impacts Black women’s experiences during pregnancy and childbirth. Preconceived notions and stereotypes can lead to inadequate or delayed diagnosis, inappropriate treatment, and a lack of empathy and cultural sensitivity. This can manifest in the form of providers exhibiting implicit bias towards Black women, leading to mistrust and diminished rapport, which in turn may impede open communication about symptoms and concerns.
This lack of trust can significantly affect the quality of care received.
Systemic Racism and Healthcare Access
Systemic racism profoundly influences healthcare access and quality for Black women. This is evidenced by historical and ongoing disparities in access to quality healthcare, leading to limited opportunities for preventative care and treatment. This systemic issue extends beyond individual provider biases and permeates healthcare systems at large, creating structural barriers to equitable care. The cumulative effect of these factors results in a lack of equitable healthcare for Black women, contributing to higher maternal mortality rates.
Comparison of Socioeconomic Factors and Maternal Mortality Rates
| Socioeconomic Factor | Impact on Maternal Mortality Rates | Example |
|---|---|---|
| Poverty | Limited access to prenatal care, nutritious food, and safe housing, increasing risk of complications. | A woman living in poverty may not be able to afford transportation to prenatal appointments. |
| Lack of Healthcare Access | Delayed or missed diagnoses, inadequate treatment of existing health conditions, increased risk of complications. | A woman with limited insurance may postpone or avoid necessary medical procedures. |
| Limited Educational Opportunities | Reduced understanding of maternal health risks and preventative measures, impacting self-advocacy within healthcare system. | A woman with limited education may have less awareness of the importance of regular prenatal check-ups. |
| Implicit Bias | Inadequate or delayed diagnosis, inappropriate treatment, lack of empathy and cultural sensitivity. | A provider might dismiss a Black woman’s pain or symptoms as non-serious. |
| Systemic Racism | Structural barriers to equitable care, including limited access to resources, culturally insensitive practices, and lack of culturally competent healthcare providers. | Lack of representation of Black women in leadership positions within healthcare institutions. |
Healthcare Access and Quality
The quality and accessibility of healthcare play a crucial role in maternal health outcomes. Disparities in these areas contribute significantly to the disproportionately high maternal mortality rate among Black women. This section delves into the specific challenges Black women face in accessing prenatal care, delivery services, and postpartum follow-up, examining the quality of care they receive and the types of providers they utilize.
Understanding these disparities is essential for developing targeted interventions to improve maternal health outcomes.Access to quality healthcare is a complex issue, interwoven with systemic factors that create unequal opportunities for Black women. The quality of care experienced by Black women is often different from that of other racial groups, reflecting broader societal biases and inequalities. This difference in care contributes to the persistent maternal mortality gap, necessitating a deeper understanding of the specific challenges and the development of equitable solutions.
Prenatal Care Disparities
Black women often experience significant barriers to accessing adequate prenatal care. These barriers may include limited financial resources, geographic location, lack of transportation, and implicit bias within the healthcare system. Insufficient access to comprehensive prenatal care can lead to delayed or missed diagnoses of complications, potentially impacting pregnancy outcomes. Further, the quality of prenatal care received may vary based on race, impacting the health and well-being of the mother and child.
Delivery Services and Postpartum Follow-up
Access to high-quality delivery services and postpartum follow-up is essential for a healthy recovery. Black women may face disparities in the type of delivery services offered and the quality of postpartum care received. Factors such as implicit bias among healthcare providers and a lack of culturally competent care can affect the type and quality of care provided, which can lead to poorer outcomes for Black women.
The lack of culturally sensitive care can negatively affect the perception of the care received by the patient, impacting the health of both the mother and child.
Quality of Healthcare Received
Studies show that Black women may experience disparities in the quality of healthcare received compared to other racial groups. This can manifest in differing diagnoses, treatment protocols, and pain management strategies. Factors like implicit bias among healthcare providers can contribute to variations in the quality of care. Differences in communication styles and cultural understanding between patients and providers can further exacerbate these issues.
Healthcare Provider Utilization
Black women’s utilization of healthcare providers, such as obstetricians/gynecologists (OBGYNs) and midwives, may differ from other racial groups. Factors such as trust, cultural familiarity, and access to providers within their communities can influence the types of providers they choose. This difference in provider choice can influence the quality and type of care received.
Implicit Bias and Cultural Competency
Implicit bias among healthcare providers can affect the quality of care provided to Black women. Implicit biases can lead to subconscious judgments and treatment disparities. A lack of cultural competency among healthcare providers can also negatively impact patient outcomes. Cultural competency in healthcare involves understanding and respecting the diverse cultural backgrounds of patients, which includes acknowledging and addressing potential biases in the system.
Healthcare providers need to be aware of how their own biases might influence their interactions with Black patients. This requires ongoing training and education to foster a more equitable healthcare system.
Correlation Table: Healthcare Access and Maternal Mortality Rates
| Type of Healthcare Access | Correlation with Maternal Mortality Rates for Black Women |
|---|---|
| Prenatal Care (adequate/timely) | Inverse correlation; adequate prenatal care reduces mortality rates |
| Delivery Services (high-quality) | Inverse correlation; high-quality care reduces complications and mortality |
| Postpartum Follow-up (comprehensive) | Inverse correlation; timely and comprehensive follow-up reduces risk of complications |
| Providers with Cultural Competency | Inverse correlation; culturally competent providers understand and address unique needs |
| Healthcare Providers with Implicit Bias Training | Inverse correlation; training reduces potential bias |
Specific Risk Factors: Childbirth Maternal Mortality Black Women

Understanding the specific risk factors contributing to adverse pregnancy outcomes and maternal mortality in Black women is crucial for developing targeted interventions. These factors often intersect with pre-existing health conditions, socioeconomic disparities, and systemic inequities within the healthcare system. Addressing these complex issues requires a multifaceted approach that considers the individual and societal contexts surrounding Black women’s health.The prevalence of certain risk factors for Black women during pregnancy, childbirth, and postpartum, often differs significantly from other racial groups.
The stark reality of childbirth maternal mortality rates among Black women is a deeply concerning issue. While the Biden administration tackles important policy decisions, like the recent veto of the Republican electric vehicle charging initiative biden veto republican electric vehicle charging , we need to remember that these broader economic and societal factors also disproportionately impact the health and well-being of this community.
Addressing this critical disparity remains a pressing priority.
This difference necessitates a nuanced approach to identifying, assessing, and managing these complications. Early detection and timely intervention are essential to improving outcomes. Recognizing these disparities allows for more proactive healthcare strategies that aim to reduce preventable maternal mortality and morbidity.
Specific Risk Factors for Adverse Pregnancy Outcomes
Several specific risk factors significantly contribute to adverse pregnancy outcomes in Black women. These include pre-existing conditions like hypertension, diabetes, and obesity, which can exacerbate pregnancy-related complications. Furthermore, inadequate access to prenatal care, delayed or infrequent prenatal visits, and limited access to quality obstetric care can all increase the risk of complications. In some cases, limited access to culturally competent healthcare providers and the unique challenges of navigating the healthcare system can also contribute to disparities.
Common Pregnancy Complications
Black women experience a higher prevalence of certain complications during pregnancy, delivery, and postpartum. These include gestational hypertension, preeclampsia, eclampsia, preterm birth, postpartum hemorrhage, and cesarean delivery. These complications can have severe consequences for both the mother and the baby, impacting long-term health and well-being. For example, preeclampsia can lead to seizures, stroke, and kidney damage, while postpartum hemorrhage can result in severe blood loss, potentially life-threatening.
Prevalence Comparison
Studies have consistently shown a higher prevalence of these complications in Black women compared to other racial groups. For instance, preterm birth rates are often significantly higher among Black women, which is a leading cause of infant mortality. This disparity highlights the urgent need for targeted interventions to address the root causes of these health disparities.
Importance of Early Detection and Management
Early detection and effective management of these complications are critical for improving outcomes. Comprehensive prenatal care, including regular check-ups, blood pressure monitoring, and blood glucose testing, can help identify potential problems early on. Prompt and appropriate interventions, such as medication management and close monitoring, can minimize the risks associated with these conditions.
Table: Specific Risk Factors and Associated Maternal Mortality Rates
| Risk Factor | Description | Associated Maternal Mortality Rate (Estimated, varies by study) |
|---|---|---|
| Pre-existing Hypertension | High blood pressure prior to pregnancy | Increased risk |
| Diabetes | Diabetes before or during pregnancy | Increased risk |
| Obesity | High body mass index (BMI) | Increased risk |
| Inadequate Prenatal Care | Limited or delayed prenatal care | Increased risk |
| Preeclampsia/Eclampsia | High blood pressure during pregnancy with protein in the urine | Significant risk |
| Postpartum Hemorrhage | Excessive bleeding after delivery | Significant risk |
| Preterm Labor | Labor before 37 weeks of gestation | Significant risk |
| Cesarean Section | Delivery by Cesarean | Increased risk if complicated |
Note: This table provides a general overview and estimated risks. Actual rates may vary based on specific circumstances and access to quality care.
Policy and Intervention Strategies
Addressing the persistent disparities in maternal mortality among Black women requires a multifaceted approach that encompasses policy changes, improved healthcare access, and community-based interventions. Existing policies, while often well-intentioned, have shown limited effectiveness in reducing the racial gap. A comprehensive strategy is needed to ensure that all pregnant Black women have access to the quality care and resources they need to achieve positive birthing outcomes.
The staggering statistics on childbirth maternal mortality rates among Black women are deeply troubling. It’s a critical issue that demands immediate attention and action. The recent cancellation of the Indiana University Samia Halaby exhibition, which unfortunately mirrors the systemic issues often hidden in plain sight, underscores the need for open conversations about these disparities and the importance of supporting Black women’s health.
This whole situation really highlights the complex challenges we face in achieving true equality and well-being for all mothers.
Existing Policies and Their Impact
Policies aimed at reducing maternal mortality often focus on expanding access to prenatal care, improving the quality of obstetric care, and addressing socioeconomic factors. However, the effectiveness of these policies in reducing racial disparities is often inconsistent and needs further improvement. The implementation of policies should be accompanied by rigorous evaluation to assess their impact and identify areas for improvement.
The stark reality of childbirth maternal mortality rates among Black women is a deeply troubling issue. While recent legal victories, like the one Thailand’s Pita won in a significant case ( thailand pita wins case ), offer hope for positive change in various areas, we must still address the systemic inequities that contribute to these disproportionately high rates.
These alarming statistics demand urgent attention and action to improve healthcare access and outcomes for Black mothers.
Strategies for Improving Access to Quality Healthcare
Ensuring equitable access to quality healthcare for Black women requires a multifaceted approach. This includes increasing the representation of Black healthcare providers in the system, creating culturally competent care environments, and promoting trust and open communication between patients and providers. Furthermore, addressing implicit bias in healthcare settings is crucial for ensuring equitable treatment and outcomes. Efforts should also focus on training healthcare providers on culturally sensitive practices and providing ongoing support to address the unique needs of Black women during pregnancy.
Community-Based Interventions
Community-based interventions play a vital role in supporting pregnant Black women and reducing maternal mortality. These interventions should empower communities to advocate for their needs, provide culturally sensitive education and support, and promote access to resources. Community health workers, trained in maternal health and cultural competency, can be instrumental in identifying and addressing potential risks early on. For example, community-based support groups could provide emotional support, practical guidance, and a platform for sharing experiences and knowledge.
The stark reality of childbirth maternal mortality rates among Black women is a deeply troubling issue. While the news cycle often focuses on sports, recent headlines about Arthur Smith being hired as the Steelers’ offensive coordinator, arthur smith hired steelers offensive coordinator , highlight the broader need for societal attention to pressing issues. The disproportionate impact on Black women demands a multifaceted approach to tackle systemic inequalities that contribute to these devastating statistics.
Peer support networks can significantly improve access to information and emotional well-being for pregnant Black women.
Table Summarizing Existing Policies and Impact
| Policy Area | Example Policy | Potential Impact on Maternal Mortality (Black Women) | Effectiveness Evaluation |
|---|---|---|---|
| Prenatal Care Access | Medicaid expansion, increased funding for community health centers | Increased access to care, potentially reduced mortality rates | Mixed results, depending on the specific policy and implementation. Further evaluation needed. |
| Obstetric Care Quality | Training programs for providers on cultural competency, implicit bias, and maternal health complications. | Improved care quality, reduced complications, potential reduction in mortality | Effectiveness varies based on program quality, provider buy-in, and ongoing monitoring. |
| Socioeconomic Factors | Targeted programs to address poverty, food insecurity, and lack of affordable housing | Reduced stress and improved health outcomes, potentially reducing mortality rates | Evaluation requires longitudinal studies and detailed tracking of outcomes. |
| Community-Based Interventions | Establishment of community health worker programs and support groups focused on maternal health | Improved knowledge, access to resources, and emotional support, potentially leading to lower mortality | Impact depends on the program’s design, community engagement, and sustainability. |
Cultural Considerations
Pregnancy and childbirth are deeply intertwined with cultural beliefs and practices. Understanding these nuances is crucial for providing culturally sensitive care to Black women, a population disproportionately affected by maternal mortality. These beliefs often shape decisions about healthcare access, birthing preferences, and overall well-being, highlighting the importance of respecting and incorporating cultural values into maternal care.Cultural factors influence the entire experience of pregnancy and childbirth for Black women, impacting their interactions with healthcare providers, their choices regarding birthing plans, and their access to support systems.
This includes a spectrum of beliefs, from traditional healing practices to societal expectations surrounding motherhood, all of which have the potential to affect health outcomes. Addressing these influences through culturally sensitive care is critical to improving maternal health outcomes and reducing disparities.
Impact of Cultural Beliefs on Healthcare Access
Cultural beliefs can significantly influence a Black woman’s decision to seek or engage with healthcare during pregnancy and childbirth. For example, some communities may have strong beliefs about the roles of family members in healthcare decisions, or may prefer traditional healers alongside or instead of conventional medical care. Respecting these choices and finding ways to integrate these practices into the care plan can improve patient trust and engagement.
Understanding the importance of family involvement in decision-making is crucial for effective communication and building trust with patients.
Culturally Sensitive Care Practices
Culturally sensitive care is essential to address the unique needs of Black women. This involves actively listening to their experiences, acknowledging and respecting their cultural values, and integrating traditional healing practices where appropriate. Such care is not merely about acknowledging differences; it’s about actively incorporating them into the healthcare framework.
- Language Access: Providing access to interpreters and materials in the languages spoken within the community can facilitate clear communication and address potential misunderstandings.
- Traditional Healing Practices: Understanding and respecting the role of traditional healers in the community, if desired by the patient, can lead to a more holistic and culturally appropriate approach to care.
- Family Involvement: Recognizing and supporting the role of family members in decision-making can foster a sense of trust and ownership in the healthcare process.
Examples of Culturally Appropriate Interventions
Various interventions can be implemented to promote culturally sensitive care. These include community health workers trained in culturally appropriate communication and support, community-based education programs addressing maternal health, and culturally relevant workshops and support groups.
- Community Health Workers: These individuals, often from the community itself, can serve as vital links between healthcare providers and expectant mothers, facilitating culturally sensitive communication and support.
- Community-Based Education: Educational programs tailored to the specific needs and cultural values of the community can empower women with knowledge about pregnancy and childbirth, fostering informed decision-making.
- Support Groups: Support groups led by community members can provide a safe space for women to share experiences, learn from each other, and receive emotional support during pregnancy and childbirth.
Comparing Cultural Practices
A comparison of cultural practices affecting maternal health outcomes for Black women versus other groups reveals unique considerations. While cultural factors influence all groups, the specific beliefs and practices that affect Black women often stem from historical and systemic factors that have contributed to disparities in healthcare access and outcomes.
“Cultural sensitivity in healthcare is not about erasing cultural differences, but about recognizing and respecting them, and using that understanding to provide more effective and appropriate care.”
Data and Research Gaps
Understanding the stark reality of maternal mortality among Black women requires a deep dive into the existing data and research. Unfortunately, the current body of knowledge, while illuminating some aspects, falls short in comprehensively capturing the multifaceted nature of this critical issue. This leaves significant gaps in our understanding, hindering the development of effective interventions and policies to address the disparity.
A critical analysis of the available data is crucial to identifying these gaps and informing future research priorities.
Existing Research on Maternal Mortality Among Black Women
Numerous studies have explored maternal mortality rates among Black women, highlighting the persistent disparity compared to other racial groups. These studies have often examined socioeconomic factors, access to healthcare, and specific risk factors contributing to this disparity. While providing valuable insights, existing research often lacks a holistic perspective, sometimes focusing on isolated factors rather than the complex interplay of these factors.
The stark reality of childbirth maternal mortality rates among Black women is a deeply troubling issue. It’s a heartbreaking statistic, highlighting the urgent need for solutions. Thinking about the resilience and strength of individuals like those featured in Holocaust survivor portraits, like those by Gillian Laub, holocaust survivor portraits gillian laub , makes me realize how crucial it is to fight for equitable healthcare and address the systemic issues contributing to these disparities.
Ultimately, we must continue to push for solutions to improve maternal health outcomes for all women.
For instance, some studies may focus on poverty without considering the role of implicit bias within the healthcare system.
Gaps in Current Data and Research
Current data on maternal mortality often lacks granular detail on the specific experiences of Black women. This includes a need for more nuanced information on socioeconomic circumstances, cultural considerations, and the specific healthcare encounters of this population. Furthermore, research frequently fails to account for the intersectional nature of these factors. For instance, the experience of a Black woman living in poverty and experiencing discrimination in the healthcare system is not adequately captured in existing research, making it challenging to understand the unique challenges she faces.
Importance of Comprehensive Data Collection and Analysis
Comprehensive data collection and analysis are essential for understanding the underlying causes of maternal mortality among Black women. This includes gathering data on not only the demographic and socioeconomic factors but also on the healthcare system’s response to their needs. This data collection should encompass various aspects, including experiences of discrimination, cultural barriers, and the quality of care received.
Such data would provide a clearer picture of the complexities and offer a foundation for more targeted interventions.
Areas for Future Research, Childbirth maternal mortality black women
Future research should prioritize a deeper understanding of the intersectional experiences of Black women. This includes studying the interaction of race, socioeconomic status, geographic location, and access to healthcare on maternal outcomes. Research should also investigate the role of implicit bias within healthcare systems and how it impacts the quality of care provided to Black women. Furthermore, studies should delve into the impact of cultural beliefs and practices on maternal health decisions.
The goal should be to develop interventions tailored to the specific needs and experiences of Black women.
Table of Current Research Findings and Highlighted Gaps
| Research Area | Current Findings | Gaps Identified |
|---|---|---|
| Socioeconomic Factors | Studies show a strong correlation between poverty and higher maternal mortality rates among Black women. | Limited research on the specific mechanisms through which socioeconomic factors impact maternal health, and a lack of data on the experiences of women in various socioeconomic strata. |
| Healthcare Access and Quality | Disparities in access to prenatal care and quality of care exist. | Insufficient data on the specific types of discrimination faced by Black women within the healthcare system, and the impact of implicit bias on healthcare outcomes. |
| Specific Risk Factors | Studies have identified certain medical conditions as risk factors for Black women. | Lack of research on the interaction of these risk factors with other factors such as socioeconomic status and healthcare access. |
| Cultural Considerations | Cultural beliefs and practices may influence maternal health decisions. | Limited data on how these considerations impact healthcare utilization and outcomes. |
Concluding Remarks
In conclusion, childbirth maternal mortality among Black women is a multifaceted problem rooted in historical injustices, socioeconomic factors, and healthcare disparities. Understanding the complexities of these issues is critical to developing effective interventions and policies to improve maternal health outcomes for Black women. We must recognize the need for culturally sensitive care, improved access to quality healthcare, and systemic changes to address the root causes of these disparities.
Commonly Asked Questions
What are some common complications experienced by Black women during pregnancy?
Black women are disproportionately affected by complications like preeclampsia, gestational diabetes, and postpartum hemorrhage. These complications, when not properly managed, can lead to severe health problems or even death.
How does implicit bias affect healthcare experiences for Black women?
Implicit bias among healthcare providers can lead to variations in treatment and care quality, impacting diagnosis, treatment recommendations, and overall patient experience for Black women. This can contribute to poorer outcomes.
What specific policies are in place to address maternal mortality among Black women?
While various policies exist, their effectiveness in reducing disparities remains a subject of ongoing discussion and research. Further analysis of existing policies and potential new initiatives is needed.
What are the data gaps in research on maternal mortality among Black women?
Further research is needed to understand the nuanced factors and the unique challenges Black women face. More comprehensive data collection, analysis, and diverse research methodologies are essential to accurately understand and address the disparities.

