
Spider Veins Telangiectasias Blood Vessels A Deep Dive
Spider veins telangiectasias blood vessels, those delicate, often unsightly, and sometimes concerning thread-like veins, are a common concern for many. This comprehensive exploration delves into the intricate world of these vascular conditions, examining their causes, diagnoses, treatments, and impact on quality of life. We’ll uncover the differences between spider veins and other related vascular issues, understand the role of genetics and lifestyle, and explore the available solutions for managing these aesthetic and sometimes health-related concerns.
From the underlying science of blood vessel function to the emotional and social impact of these veins, we’ll paint a detailed picture of spider veins. Understanding the nuances of spider vein telangiectasias blood vessels is key to navigating treatment options and preventative measures.
Introduction to Spider Veins and Telangiectasias
Spider veins, also known as telangiectasias, are small, dilated blood vessels that appear as reddish or bluish lines, webs, or clusters on the skin. They are a common cosmetic concern, often appearing on the legs, face, and other areas. These delicate vessels are superficial and typically harmless, although they can sometimes indicate underlying health conditions.Telangiectasias differ from other vascular conditions like varicose veins, which are larger, more prominent, and often cause discomfort.
Varicose veins involve the deeper veins, while spider veins affect the smaller, superficial capillaries. Furthermore, while spider veins can occur in various situations, varicose veins usually involve a structural problem within the vein’s valves or walls. Distinguishing these conditions helps in appropriate diagnosis and treatment.
Typical Appearance and Location
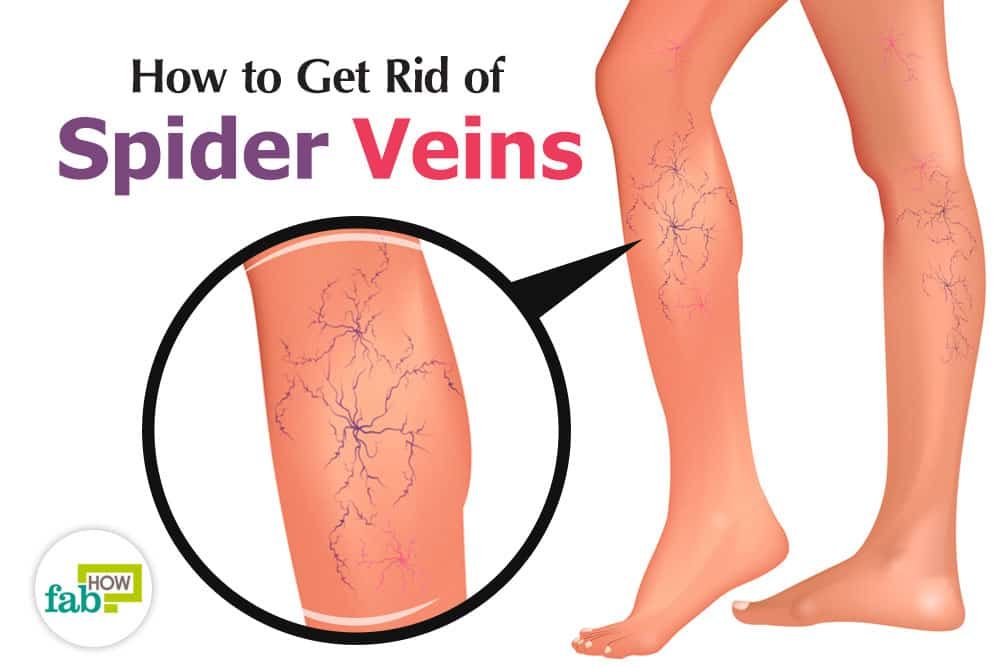
Spider veins typically appear as small, thread-like or branching lines of red, purple, or blue, resembling a spider’s web. Their appearance varies depending on the individual and the location. They frequently occur on the legs, especially the ankles and lower shins, but can also develop on the face, neck, and arms. Their size can range from a few millimeters to a few centimeters in diameter.
Spider veins, also known as telangiectasias, are those tiny, visible blood vessels that can show up on your legs or face. Figuring out the best approach to treat them can be tricky, but understanding the underlying causes is a good starting point. Knowing how to choose the right treatment for these blood vessel issues can also be important for your overall health.
While we’re on the topic of family matters, learning about the rules surrounding the last name of a child, like apellido bebe madre padre , can be just as important as understanding the causes and treatments of spider veins. Ultimately, whether you’re dealing with inheritance laws or improving your appearance, taking care of your health is key.
Common Causes of Spider Veins
Several factors contribute to the development of spider veins, including genetics, hormonal changes, and lifestyle choices. Heredity plays a significant role, with individuals having a predisposition to spider veins being more likely to develop them. Hormonal fluctuations, such as those associated with pregnancy or menopause, can also influence the appearance of spider veins. Certain medications, prolonged standing or sitting, and sun exposure can also contribute to their formation.
Spider veins, or telangiectasias, are those tiny, often reddish or purplish blood vessels that can show up on the skin. While they’re mostly harmless, they can be a bit unsightly. Sometimes, the complexities of wealth and high-stakes dealings, like in the recent Rybolovlev v. Sotheby’s art fraud trial rybolovlev sothebys art fraud trial , can lead to surprising and even intricate problems.
Ultimately, though, the beauty of the skin and the health of the blood vessels underneath are still important.
Types of Spider Veins
| Type | Description | Location | Cause |
|---|---|---|---|
| Reticular Veins | These are larger than spider veins, appearing as a network of fine, slightly raised lines. | Legs, especially lower legs | Genetic predisposition, prolonged standing, hormonal changes, and pregnancy. |
| Spider Veins (Telangiectasias) | These are the most common type, characterized by small, branching, thread-like lines or clusters of dilated blood vessels. | Legs, face, and sometimes the arms | Hormonal changes, genetics, sun exposure, and certain medications. |
| Rosacea-Associated Spider Veins | These are spider veins that develop in individuals with rosacea, a chronic skin condition characterized by facial redness and inflammation. | Face, particularly the cheeks, nose, and forehead | Rosacea, often in combination with other factors like sun exposure and genetics. |
| Post-inflammatory Spider Veins | These are spider veins that appear after skin injury or inflammation. | Face and body, wherever inflammation or injury occurred. | Trauma, burns, and skin conditions that cause inflammation. |
Causes and Risk Factors
Spider veins, or telangiectasias, aren’t just an aesthetic concern; understanding their causes and risk factors is crucial for prevention and treatment. While some factors are unavoidable, knowledge empowers individuals to make informed choices about their lifestyle and health. Many people find that addressing these factors can make a noticeable difference in managing spider vein appearance.Genetics play a significant role in predisposition to spider veins.
Spider veins, also known as telangiectasias, are those tiny, visible blood vessels that can sometimes appear on the skin. While they’re often harmless, they can be quite noticeable, especially in women. Interestingly, some research suggests that a fit and active lifestyle, like that of the women playing in the Women’s Professional Hockey League (WPHL) in New York womens hockey pwhl new york , might contribute to overall circulation and potentially minimize the appearance of these blood vessels.
However, it’s important to remember that various factors can influence spider vein formation. Ultimately, consulting a dermatologist is key for proper diagnosis and treatment options.
If family members have a history of these veins, the likelihood of developing them increases. This genetic predisposition often manifests as a tendency toward thinner blood vessel walls, which makes them more susceptible to dilation. Hormonal fluctuations, particularly during pregnancy or menopause, can also lead to increased blood flow and pressure in the veins, further contributing to spider vein development.
Genetics and Spider Vein Formation
Inherited traits, such as the structure and strength of blood vessel walls, can significantly influence a person’s susceptibility to spider veins. Individuals with a family history of spider veins often have a higher risk of developing them themselves. This is often due to genetic variations affecting collagen and elastin production, which are crucial for maintaining healthy blood vessel integrity.
Spider veins, or telangiectasias, are those tiny, red or blue blood vessels that can sometimes appear on the skin. While they’re often harmless, they can be frustrating. Speaking of frustrating, I just saw the Oilers beat the Blue Jackets, thanks to a clutch performance by Stuart Skinner oilers stuart skinner defeat blue jackets. Good game, but nothing beats getting those spider veins treated, especially if they’re causing discomfort or concern.
Still, it’s important to keep an eye on them, and consider talking to a dermatologist if needed.
Hormonal Changes and Spider Vein Development
Hormonal shifts throughout a woman’s life, such as during pregnancy and menopause, can significantly impact blood vessel health. Fluctuations in estrogen levels, for instance, can affect blood flow and pressure, potentially leading to the dilation of capillaries and the formation of spider veins. Increased blood volume during pregnancy also places additional stress on the circulatory system, increasing the risk of spider vein development.
Sun Exposure and Spider Veins
Prolonged and intense sun exposure can contribute to spider vein formation. Ultraviolet (UV) radiation can damage blood vessels, making them more susceptible to dilation and the appearance of spider veins. Sun-exposed areas, like the legs and face, are more prone to developing these veins due to increased exposure.
Pregnancy and Age: Effects on Spider Vein Appearance
Pregnancy and aging are both associated with spider vein development, although their impacts differ. During pregnancy, the increased blood volume and hormonal changes increase pressure on blood vessels, contributing to their dilation. As individuals age, the skin’s elasticity naturally decreases, potentially leading to a greater likelihood of spider veins forming. This is particularly true in sun-exposed areas.
Lifestyle Factors Increasing Spider Vein Risk
Several lifestyle choices can influence the risk of developing spider veins. These include:
- Prolonged Standing or Sitting: Standing or sitting for extended periods can increase pressure on the veins in the legs, potentially leading to dilation and spider vein formation.
- Obesity: Excess weight can put extra strain on the circulatory system, increasing the risk of spider veins.
- Tight Clothing: Tight clothing, especially around the legs, can restrict blood flow, increasing pressure on the veins and potentially contributing to spider vein development.
- Lack of Physical Activity: A sedentary lifestyle can negatively affect circulation, increasing the risk of spider veins.
- Dehydration: Insufficient water intake can lead to thicker blood, increasing the strain on blood vessels and potentially contributing to spider vein formation.
Diagnosis and Evaluation
Pinpointing the cause of spider veins, or telangiectasias, is crucial for effective treatment. A thorough diagnostic process involves a combination of visual assessments and sometimes, medical imaging. This allows healthcare professionals to understand the extent of the condition and tailor the most suitable treatment plan for each individual.
Physical Examination
A physical examination is the cornerstone of spider vein diagnosis. The process begins with a careful visual inspection of the affected area. The doctor will look for the characteristic dilated, superficial blood vessels that are the hallmark of spider veins. This visual evaluation helps to assess the size, distribution, and number of spider veins. The doctor might also feel the area to evaluate for any associated inflammation or tenderness, which could point to underlying conditions.
These examinations allow for an initial assessment of the severity and extent of the spider veins.
Role of Medical Imaging
While a physical examination is often sufficient, medical imaging plays a supportive role in certain cases. Imaging techniques like ultrasound are occasionally used to determine the depth and structure of the blood vessels involved. Ultrasound can help differentiate between spider veins and other conditions that may present with similar visual characteristics. For example, if a patient presents with skin discoloration that mimics spider veins, an ultrasound could help differentiate between the two.
Ultrasound helps in precise diagnosis, particularly when the spider veins are deep or when there’s a suspicion of underlying vascular abnormalities.
Diagnostic Pathway Flowchart
The following table Artikels a typical diagnostic pathway for spider veins. This structured approach helps ensure a comprehensive evaluation and guides the treatment process.
| Step | Description | Procedure | Result |
|---|---|---|---|
| 1 | Patient history and initial evaluation | Detailed discussion of symptoms, medical history, family history, and lifestyle factors. Visual inspection of the affected area. | Identification of potential risk factors, confirmation of spider vein presence, and initial assessment of severity. |
| 2 | Physical Examination | Careful visual inspection of the affected area, palpation for tenderness or inflammation, and assessment of spider vein characteristics (size, distribution, number). | Confirmation of spider vein diagnosis, assessment of their distribution and extent. |
| 3 | Diagnostic Imaging (Optional) | Ultrasound imaging of the affected area, potentially to evaluate the depth and structure of the blood vessels. | Confirmation of spider vein characteristics, differentiation from other conditions, or evaluation of underlying vascular abnormalities. |
| 4 | Differential Diagnosis | Comparison of findings with other potential conditions that may present with similar symptoms. | Final diagnosis of spider veins and exclusion of other conditions. |
Treatment Options
Dealing with spider veins, or telangiectasias, can be a frustrating experience. Fortunately, a range of effective treatments are available, addressing various needs and preferences. The best approach depends on the severity of the condition, the patient’s overall health, and their individual goals. Understanding the different treatment options, their mechanisms of action, and potential risks can empower individuals to make informed decisions about their care.
Overview of Treatment Methods
Various treatment options exist for spider veins, ranging from minimally invasive procedures to more traditional approaches. The choice of treatment often depends on the size, number, and location of the affected veins. A healthcare professional can evaluate the specific situation and recommend the most appropriate method.
Sclerotherapy
Sclerotherapy is a common and effective treatment for spider veins. This procedure involves injecting a sclerosing solution directly into the affected veins. The solution irritates the vein walls, causing them to collapse and eventually disappear. The body then absorbs the collapsed veins. This minimally invasive technique often requires multiple sessions to achieve optimal results.
Laser Therapy
Laser therapy uses concentrated light beams to heat and destroy the spider veins. The heat causes the veins to collapse, and the body eventually absorbs them. Laser treatments can be effective for smaller spider veins, but larger or more extensive veins might require additional treatments. Laser therapy often provides faster results and minimal discomfort compared to other methods.
Surgical Procedures
Surgical procedures are typically reserved for more severe cases of spider veins or when other treatments have failed. These procedures involve surgically removing the affected veins. While effective, they usually involve more significant recovery time and potential risks compared to minimally invasive methods.
Comparison of Treatment Methods
| Method | Cost | Recovery Time | Efficacy |
|---|---|---|---|
| Sclerotherapy | Moderate to High | Generally short, days to weeks | High, but multiple sessions often needed |
| Laser Therapy | Moderate to High | Generally short, days to weeks | High, especially for smaller veins |
| Surgical Procedures | High | Longer, weeks to months | High, but usually for more severe cases |
Potential Risks and Side Effects
All treatment options for spider veins carry potential risks and side effects. Sclerotherapy may cause bruising, pain, or redness at the injection site. Laser therapy can lead to temporary skin discoloration or discomfort. Surgical procedures carry the risk of infection, scarring, or complications related to anesthesia. It’s crucial to discuss these potential risks with a healthcare professional before making a decision.
Individual responses to treatment can vary. Some individuals might experience minimal side effects, while others might experience more pronounced reactions.
Prevention Strategies
Spider veins, or telangiectasias, can be frustrating and sometimes even embarrassing. While there’s no guaranteed way to prevent them entirely, proactive measures can significantly reduce your risk. Understanding the contributing factors and adopting a healthy lifestyle are key to minimizing the appearance of these delicate blood vessels.
Lifestyle Choices for Prevention
Maintaining a healthy lifestyle plays a crucial role in preventing spider vein development. Certain habits and choices can contribute to the formation of these veins, while others can actively mitigate the risk. These include dietary habits, exercise routines, and sun protection strategies.
- Healthy Weight Management: Maintaining a healthy weight is essential for overall vascular health. Excess weight puts extra strain on blood vessels, increasing the risk of developing spider veins. A balanced diet and regular exercise are crucial components of weight management and overall well-being. For instance, someone who loses 10-15 pounds through a combination of diet and exercise might experience a noticeable reduction in spider vein visibility.
- Sun Protection: Prolonged sun exposure can weaken the walls of blood vessels, making them more prone to dilation and the formation of spider veins. Using sunscreen with a high SPF (30 or higher) and protective clothing, especially during peak sun hours, is essential for protecting your skin and minimizing the risk of spider veins.
- Regular Exercise: Regular physical activity strengthens the circulatory system and improves blood flow. This can help maintain healthy blood vessel tone and reduce the risk of spider vein formation. Activities like walking, swimming, or cycling can significantly contribute to this. For example, individuals who engage in regular 30-minute walks three times a week often experience improved circulation and a reduced risk of spider veins.
Compression Stockings: A Preventive Tool
Compression stockings provide gentle support to the veins in the legs, helping to improve blood flow and reduce the pooling of blood, a key factor in spider vein formation. Choosing the right compression stockings is essential for maximizing their preventive benefits.
Compression stockings can help prevent spider vein development by promoting better blood flow and reducing pooling in the legs.
Selecting the Right Compression Stockings
Selecting the correct compression stockings is crucial for their effectiveness and comfort. Several factors should be considered.
| Factor | Explanation |
|---|---|
| Compression Level | Compression stockings are categorized by their level of compression (e.g., low, medium, high). The appropriate level depends on individual needs and conditions. Consult with a healthcare professional or a qualified retailer for guidance. |
| Material and Fit | Look for comfortable, breathable materials like nylon or spandex. The stockings should fit snugly but not tightly, ensuring proper compression without constriction. Proper fit avoids discomfort or potential skin irritation. |
| Medical Advice | Consulting with a doctor or a certified medical professional can help in choosing the correct compression level and type of stockings, tailored to individual needs and circumstances. They can assess your specific situation and recommend the most suitable option. |
Blood Vessels and Their Role
Spider veins, or telangiectasias, are often a cosmetic concern, but understanding the underlying blood vessels is key to understanding their formation and potential treatments. This section delves into the anatomy and function of the blood vessels involved, highlighting the link between blood flow dynamics and spider vein development.
Anatomy of Blood Vessels Relevant to Spider Veins
The blood vessel network in the affected area plays a crucial role in spider vein formation. Capillaries, venules, and veins are the primary vessels involved, and their structure and function directly impact the likelihood of developing spider veins. Spider veins typically stem from superficial veins, meaning those closer to the skin’s surface.
Function of Capillaries, Venules, and Veins
Capillaries are the smallest blood vessels, forming a network throughout the body. Their thin walls facilitate the exchange of oxygen, nutrients, and waste products between the blood and surrounding tissues. Venules collect blood from capillaries, acting as small veins. Veins carry deoxygenated blood back to the heart, aided by valves that prevent backflow. The delicate balance of blood pressure and the integrity of these vessels is essential for optimal blood flow and preventing abnormalities like spider veins.
Relationship Between Blood Flow and Spider Vein Formation
Spider veins are often associated with impaired blood flow in the superficial veins. Factors such as weakened vessel walls, increased pressure in the veins, or insufficient valve function can lead to blood pooling and the development of visible dilated vessels. This pooling can be a result of increased pressure or insufficient venous return, which occurs when the valves in the veins don’t function correctly.
For example, prolonged standing or sitting can increase pressure in the legs and contribute to the formation of spider veins. Genetic predisposition can also influence the structure and function of blood vessels, increasing susceptibility to spider veins.
Impact of Blood Pressure on Spider Vein Development
Blood pressure, particularly venous pressure, significantly influences spider vein formation. Increased venous pressure can cause the delicate walls of the superficial veins to stretch and become dilated. Factors that increase venous pressure, like pregnancy, hormonal changes, and prolonged standing, can contribute to the development of spider veins. For instance, pregnancy-related hormonal changes can affect blood vessel tone and increase the risk of spider vein formation.
In some cases, high blood pressure (hypertension) may also contribute, although this is not the primary cause in most instances.
Blood Vessel Network Diagram
| Vessel Type | Function | Location | Relationship to Spider Veins |
|---|---|---|---|
| Capillaries | Exchange of oxygen, nutrients, and waste | Throughout the body’s tissues | Part of the network, not directly involved in spider vein formation |
| Venules | Collect blood from capillaries | Connecting capillaries to veins | Contribute to the overall blood flow dynamics |
| Veins | Carry deoxygenated blood back to the heart | Beneath the skin’s surface, particularly in the legs and face | Weakening or dilation of veins can lead to spider vein formation |
Impact on Quality of Life: Spider Veins Telangiectasias Blood Vessels

Spider veins, while often a cosmetic concern, can significantly impact a person’s quality of life. Beyond the visual aspect, these small, dilated blood vessels can trigger emotional and psychological distress, impacting self-esteem, social interactions, and even daily activities. Understanding these effects is crucial for comprehensive care and treatment.
Emotional and Psychological Impact, Spider veins telangiectasias blood vessels
Spider veins can evoke feelings of self-consciousness, embarrassment, and even anxiety. The perceived imperfections can lead to feelings of inadequacy and negatively impact self-esteem. Individuals may experience body image issues, particularly when the veins are prominent or located in visible areas. This can affect their confidence in social situations and hinder their enjoyment of activities.
Spider veins, also known as telangiectasias, are those tiny, red or blue blood vessels that can appear on the skin. While they’re often harmless, they can sometimes be a cosmetic concern. Recently, the political climate has been buzzing with the Haley memo in New Hampshire, raising some interesting questions about the future of the Republican party.
Regardless of the political implications, understanding and addressing these unsightly blood vessels can be quite important for many people.
Impact on Self-Esteem and Body Image
The visibility of spider veins can lead to a decline in self-esteem. This is especially true for individuals who place high value on physical appearance. Spider veins can cause feelings of shame and insecurity, making them reluctant to wear certain clothing or participate in activities where their legs are exposed. Body image concerns can manifest as avoidance of social situations or a decreased desire to engage in activities that were previously enjoyed.
Social Implications
Spider veins can affect social interactions and relationships. Individuals may feel self-conscious about their appearance, leading to avoidance of social gatherings or activities where they feel exposed. This can impact their social circles and limit their opportunities for interaction. The impact is particularly significant in situations where the veins are prominent, affecting their comfort and confidence in social settings.
Impact on Daily Activities
Spider veins can affect daily activities in subtle yet noticeable ways. For example, individuals might experience discomfort or pain, especially in warm weather or after prolonged standing. This can limit their ability to participate in activities that involve extended periods of standing or walking. They might avoid activities that could worsen their discomfort, reducing their overall physical activity and potentially affecting their health.
Coping Mechanisms
Individuals cope with spider veins in diverse ways. Some embrace acceptance, focusing on their overall well-being and choosing to live comfortably. Others seek professional advice, exploring various treatment options, to improve their appearance and alleviate discomfort. Some individuals may use makeup to camouflage the veins, while others choose to focus on other aspects of their physical and emotional well-being, like diet and exercise.
The coping mechanism chosen often depends on the individual’s personality, cultural background, and personal values.
Illustrative Examples
Spider veins, or telangiectasias, can affect anyone, and understanding their development and treatment response can be valuable. This section will delve into a case study to illustrate the process and outcomes of spider vein treatment. We will also look at different types of spider veins on various parts of the body.
A Case Study: Sarah’s Journey with Spider Veins
Sarah, a 40-year-old woman, noticed small, reddish-purple spider veins on her legs, particularly around her ankles and inner thighs. She initially attributed them to her pregnancy years ago, but they had persisted and gradually increased in number and size. This illustrates a common scenario where spider veins, though sometimes linked to pregnancy, can develop and worsen over time.
Stages of Spider Vein Development in Sarah’s Case
Sarah’s spider veins progressed through several stages. Initially, they appeared as small, delicate lines, barely noticeable. Over time, they became more prominent, exhibiting a branching pattern, and intensified in color, from a light reddish hue to a deeper, more purple shade. This gradual progression is typical of spider vein development, where initial small vessels become larger and more visible over time.
Sarah’s Treatment Method and Experience
Sarah chose sclerotherapy, a minimally invasive procedure. During the treatment, a solution was injected into the affected spider veins, causing them to collapse and eventually disappear. The procedure was performed in a doctor’s office, and Sarah experienced minimal discomfort, primarily a slight stinging sensation during the injections. She was advised to avoid strenuous activity for a few days following the treatment.
Sarah’s Response to Treatment
Sarah’s response to sclerotherapy was positive. Within a few weeks, the spider veins on her legs started to fade, and within several months, most of them had significantly reduced in size and visibility. The treatment was effective in addressing her concerns, and she reported a significant improvement in her self-esteem and confidence. She also noted that the treatment area became smoother.
Spider Vein Appearance on Different Body Parts
Spider veins, or telangiectasias, can manifest on various body parts, each presenting slightly different characteristics.
- Face: Spider veins on the face typically appear as small, thread-like, reddish-purple vessels, often concentrated around the nose, cheeks, and forehead. They can be subtle or quite prominent. The pattern can vary, from single, isolated vessels to clusters of small, radiating lines.
- Legs: Spider veins on the legs, a common location, often appear as branching, reddish-purple or bluish-red patterns, especially on the inner thighs, calves, and ankles. They can range in size from very small, fine lines to larger, more noticeable clusters.
- Hands: Spider veins on the hands, although less frequent, can appear as delicate, reddish-purple lines, primarily on the back of the hands and fingers. Their size and pattern are typically less pronounced compared to those on the face or legs.
Image Descriptions (Illustrative examples)
Visualizing spider veins can help in understanding their appearance and characteristics. Imagine a network of tiny, red or purple threads, like a spider’s web, on the affected area. The veins may appear clustered together or as isolated, thin lines. On the legs, the pattern might resemble a starburst or a network of lines spreading outward. On the face, the veins might appear as small, reddish-purple lines radiating from a central point.
Remember that the exact appearance can vary depending on the individual and the location.
End of Discussion

In conclusion, spider veins telangiectasias blood vessels are a complex issue influenced by various factors. From genetics to lifestyle, the development and management of these conditions require a holistic approach. This exploration highlights the importance of seeking professional guidance and understanding the full spectrum of options available to address these veins. By arming ourselves with knowledge, we can better understand and manage spider veins and their impact on our well-being.
Helpful Answers
What are the most common locations for spider veins?
Spider veins frequently appear on the legs, face, and ankles, but they can also appear on the arms and chest.
Are spider veins painful?
Generally, spider veins are not painful, though some individuals may experience mild discomfort or itching.
Can spider veins be prevented?
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and sun protection, can help minimize the risk of developing spider veins.
What are the different treatment options for spider veins?
Treatment options range from topical creams and lifestyle changes to sclerotherapy, laser treatments, and surgical procedures.

