Death Medical Aid in Dying A Comprehensive Guide
Death medical aid in dying is a complex and sensitive issue, raising profound ethical and legal questions. This guide explores the multifaceted nature of medical aid in dying (MAID), examining its definition, patient eligibility, medical procedures, ethical implications, and the crucial support systems in place for those facing end-of-life decisions. We’ll delve into the legal frameworks across various jurisdictions and the evolving societal impact of this practice.
This in-depth exploration will guide readers through the intricate process of medical aid in dying, providing a comprehensive understanding of the considerations involved. We will analyze the various perspectives and provide a nuanced understanding of the topic, addressing frequently asked questions and dispelling common misconceptions.
Defining Medical Aid in Dying
Medical aid in dying (MAID) is a complex and emotionally charged issue, encompassing the provision of medical assistance to individuals who are experiencing unbearable suffering from a terminal illness. Understanding its nuances, particularly its distinction from physician-assisted suicide (PAS), is crucial for navigating the ethical and legal landscape surrounding this sensitive practice. The varying legal frameworks and eligibility criteria across different jurisdictions highlight the multifaceted considerations involved.MAID is a deliberate act of medical assistance that respects patient autonomy and enables individuals to control their final moments with dignity.
The debate around death with medical aid in dying is complex, often bringing up deeply personal feelings. Recently, the news of Chris Young’s charges being dropped, as detailed in this article chris young charges dropped , highlights the potential for legal and ethical dilemmas when considering assisted death. This case, while separate, reminds us of the profound impact such decisions can have on families and individuals, and further fuels the conversation about end-of-life care and choices.
It aims to alleviate severe suffering, recognizing the inherent value of a person’s life and their right to make choices about their own end-of-life care. The process is often meticulously regulated and involves careful evaluation to ensure that the patient’s decision is informed and voluntary.
Definition of Medical Aid in Dying
Medical aid in dying (MAID) is a practice where a physician provides medication to a competent adult patient with a grievous and irremediable medical condition to end their life at their voluntary and informed request. Key distinctions exist between MAID and physician-assisted suicide (PAS).
Distinction Between MAID and Physician-Assisted Suicide (PAS)
While both MAID and physician-assisted suicide (PAS) involve medical professionals providing assistance in hastening death, there are crucial differences. MAID involves a physician providing the means for the patient to self-administer the medication, whereas PAS involves the physician directly administering the lethal medication. Furthermore, MAID requires a specific set of criteria, including the patient’s terminal illness, and is often more strictly regulated.
Legal and Ethical Considerations Surrounding MAID
Legal and ethical considerations surrounding MAID are multifaceted and involve careful balancing of competing values. Concerns arise regarding potential coercion, safeguards for vulnerable populations, and the integrity of the medical profession. The legal frameworks surrounding MAID often address issues such as patient competency, informed consent, and the role of medical professionals in end-of-life decisions. These frameworks are designed to ensure that the patient’s choice is truly voluntary and reflects their informed understanding of the implications.
Comparison of MAID Practices Across Jurisdictions
MAID practices vary significantly across jurisdictions. For example, Canada’s approach emphasizes patient autonomy and considers factors like the patient’s unbearable suffering and prognosis. In contrast, the Netherlands has a more established history with similar but subtly different criteria. These differences reflect differing cultural values and societal priorities regarding end-of-life care.
Legal Requirements for MAID in Different Countries
The following table Artikels the key legal requirements for MAID in several jurisdictions. These criteria often include the patient’s terminal condition, the nature of the suffering, and the involvement of independent medical professionals in the decision-making process.
| Country | Eligibility Criteria | Required Physician Involvement | Timeframe Restrictions |
|---|---|---|---|
| Canada | Competent adult with a grievous and irremediable medical condition, experiencing unbearable suffering, and making a voluntary request. | Two independent medical assessments are required. | A waiting period, often 10 days, between the initial request and the administration of the medication. |
| Netherlands | Competent adult with a grievous and irremediable medical condition, experiencing unbearable suffering, and making a voluntary request. | Two independent medical assessments are required. | A waiting period is usually present. |
| Belgium | Competent adult with a grievous and irremediable medical condition, experiencing unbearable suffering, and making a voluntary request. | Two independent medical assessments are required. | A waiting period is typically present. |
Patient Eligibility and Decision-Making

Medical Aid in Dying (MAID) is a deeply personal and complex process. Understanding the criteria for eligibility and the meticulous decision-making process is crucial for ensuring that patients make informed choices in alignment with their values and circumstances. It’s important to remember that MAID is not a simple procedure, but a carefully considered option for individuals facing irreversible and unbearable suffering.The eligibility criteria and decision-making process are designed to safeguard patients from coercion and ensure that their choices are truly voluntary.
This framework emphasizes patient autonomy while maintaining ethical and legal boundaries.
Discussions around death with medical aid in dying are complex and often deeply personal. Recent headlines about the Carroll verdict and its potential impact on Haley Trump’s future highlight the intricate interplay between legal precedent and individual choices. This case, as well as the wider debate surrounding assisted death, reminds us that the right to choose how we face our final moments is a delicate balance, often influenced by legal decisions like the one surrounding Carroll verdict Haley Trump.
Ultimately, the conversation about medical aid in dying needs to acknowledge the diverse perspectives and experiences involved.
Factors Considered in Assessing Patient Eligibility
Eligibility for MAID is not automatic. Specific criteria are meticulously assessed to ensure the patient’s well-being and the appropriateness of the request. These factors typically include:
- Diagnosis of a grievous and irremediable medical condition: The condition must be confirmed by a medical professional and deemed incurable, with no reasonable hope of improvement.
- Ongoing and unbearable suffering: The patient’s pain and suffering must be of such severity that it cannot be alleviated through available medical treatments. This often involves careful consideration of the patient’s subjective experience and quality of life.
- Mental capacity: The patient must be capable of making an informed decision. This assessment often involves evaluating the patient’s understanding of their condition, prognosis, and treatment options, as well as their ability to communicate their wishes.
- Voluntariness of the request: The patient’s request must be freely and voluntarily made, without external pressure or influence from others. A crucial element is to rule out coercion or undue influence.
- Advanced care planning (if applicable): If the patient has completed advance directives or other documents outlining their wishes regarding end-of-life care, these documents are considered in the eligibility process.
Informed Decision-Making Process
A comprehensive and compassionate process is vital for ensuring that patients understand the implications of their choice. This process typically involves:
- Multiple consultations with healthcare professionals: The patient must meet with multiple physicians and other medical professionals to discuss their condition, prognosis, and treatment options. This includes the possibility of palliative care and pain management.
- Review of the patient’s medical history and current condition: A thorough review of the patient’s medical records is conducted to ensure that the assessment of their condition is accurate and comprehensive.
- Explanation of potential risks and benefits: The patient is thoroughly informed about the potential risks and benefits of MAID, including the potential side effects and the possibility of alternative treatment options.
- Support from family and friends: Family and friends can play a vital role in the process, offering emotional support and assistance in the decision-making process.
- Opportunity for reflection and discussion: The patient should have sufficient time to reflect on their decision and discuss it with loved ones, counselors, and medical professionals. This timeframe should be sufficient to address concerns and allow the patient to make a decision that aligns with their values.
Role of Mental Health Professionals
Mental health professionals play a crucial role in ensuring the patient’s psychological well-being and capacity to make an informed decision. Their role includes:
- Evaluating the patient’s psychological state: Mental health professionals assess the patient’s psychological well-being and capacity to make an informed decision. This involves identifying potential biases or influences that could affect the decision.
- Providing counseling and support: Mental health professionals can offer counseling and support to the patient and their family throughout the MAID process.
- Addressing potential underlying mental health conditions: If a mental health condition is suspected or identified, appropriate treatment is pursued to ensure the patient’s well-being.
Informed Consent and Potential for Coercion, Death medical aid in dying
Ensuring informed consent is paramount in the MAID process. The patient must be fully aware of the implications of their choice, free from coercion or undue influence.
| Step | Description |
|---|---|
| 1 | Initial Consultation and Assessment: A detailed assessment of the patient’s medical condition, psychological state, and understanding of MAID. |
| 2 | Discussion and Explanation: Comprehensive explanation of MAID, including potential risks, benefits, and alternatives. |
| 3 | Independent Review and Confirmation: Review by another physician or mental health professional to confirm the patient’s eligibility and decision-making capacity. |
| 4 | Consent Form and Documentation: The patient signs a legally binding consent form, acknowledging their understanding of the procedure and its implications. |
| 5 | Follow-up and Monitoring: Ongoing monitoring of the patient’s well-being and confirmation that the decision remains voluntary. |
The Medical Role in MAID
Medical aid in dying (MAID) is a complex process requiring careful consideration and adherence to strict medical protocols. The physician’s role is not merely to prescribe a lethal medication; it involves a comprehensive evaluation, counseling, and ongoing support for the patient. This crucial medical role necessitates adherence to ethical guidelines and legal frameworks to ensure patient safety and well-being throughout the process.The medical role in MAID encompasses a range of responsibilities, from initial evaluation to the actual administration of the medication.
It’s essential for the physician to act as a guide and support system for the patient, ensuring their comfort and understanding throughout this difficult time. The physician’s commitment to the patient’s well-being is paramount, and a careful, compassionate approach is critical to the successful and ethical execution of MAID.
Thinking about death and medical aid in dying can be really tough, but it’s important to consider all perspectives. It’s a complex issue, and sometimes personal choices regarding family matters, like determining a baby’s last name (e.g., apellido bebe madre padre ), can be just as deeply felt and challenging. Ultimately, these decisions are deeply personal, and choices surrounding medical aid in dying need to be made with care and consideration for all involved.
Physician’s Role in Providing Medical Aid in Dying
The physician plays a pivotal role in MAID, acting as a guide and supporter throughout the process. This role extends beyond simply prescribing medication; it involves comprehensive assessments, counseling, and ongoing support. Physicians must ensure the patient understands the implications of their choice and that it is made freely and voluntarily. Crucially, physicians must be knowledgeable about the patient’s medical history and current condition, including any potential risks and complications associated with MAID.
Medical Procedures Involved in MAID
The medical procedures involved in MAID are carefully defined and regulated to ensure patient safety and efficacy. The process typically involves several key steps. First, a thorough evaluation of the patient’s medical condition and psychological state is conducted. This is followed by counseling sessions to ensure the patient fully understands the process and its implications. Subsequently, the physician discusses the patient’s wishes and concerns, confirming their understanding of the procedure.
The final stage involves administering the prescribed medication in a manner consistent with the established protocols.
Required Medical Evaluations and Assessments for MAID
Thorough medical evaluations and assessments are essential to ensure the patient’s eligibility for MAID and the safety of the procedure. These evaluations typically include a detailed medical history review, a physical examination, and a psychological assessment. Furthermore, the patient’s prognosis and the presence of any underlying conditions must be considered. The assessments also aim to ascertain if the patient has a grievous and irremediable medical condition, experiencing unbearable suffering, and has made a voluntary and informed decision.
Discussions around death with medical aid in dying are always complex. Recent news regarding the Haley memo in New Hampshire, specifically the haley memo new hampshire , is raising important questions about the practical application of these laws. Ultimately, the goal of these conversations is to navigate the difficult decisions surrounding end-of-life care, and ensure compassionate choices for individuals.
Types of Medical Conditions Where MAID Might Be Considered
The applicability of MAID varies depending on the specific medical condition and the patient’s circumstances. The following table provides examples of medical conditions where MAID might be considered:
Ethical and Societal Implications: Death Medical Aid In Dying
Medical Aid in Dying (MAID) presents a complex web of ethical and societal considerations, challenging deeply held beliefs about life, death, and the role of healthcare. Navigating these complexities requires careful consideration of diverse perspectives and potential impacts on individuals, families, and healthcare systems. This exploration delves into the ethical arguments surrounding MAID, its societal effects, and the vulnerabilities inherent in its implementation.MAID’s introduction into healthcare necessitates a comprehensive examination of the ethical principles involved.
Different cultures and philosophical traditions hold varying viewpoints on the sanctity of life, the role of suffering, and the right to self-determination. These differing perspectives influence opinions on MAID, creating a dynamic interplay between individual rights and societal well-being.
Ethical Considerations
Various ethical frameworks provide different lenses through which to view MAID. Philosophical viewpoints on the value of life, the right to self-determination, and the concept of beneficence play crucial roles in shaping the debate. Respect for patient autonomy is a cornerstone of ethical MAID practice, acknowledging the patient’s right to make choices about their own end-of-life care. However, this autonomy must be balanced against potential risks and vulnerabilities.
Societal Impact
MAID’s introduction into healthcare systems has broad societal implications. Concerns exist regarding potential impacts on healthcare resources, the burden on healthcare professionals, and the possibility of abuse or coercion. The impact of MAID on end-of-life care practices, palliative care, and the overall approach to death and dying within society needs careful consideration. Changes in societal attitudes toward death and dying are often influenced by the implementation of MAID.
Different Viewpoints on MAID
Diverse viewpoints exist regarding MAID, ranging from strong support for patient autonomy and relief from suffering to concerns about potential risks and societal consequences. Supporters emphasize the importance of individual choice and the right to a dignified death, highlighting the alleviation of suffering as a crucial component. Opponents, however, raise concerns about potential coercion, the sanctity of life, and the potential for misuse of the law.
Potential Vulnerabilities and Risks
The MAID process inherently involves vulnerabilities, including the potential for coercion, undue influence, or inadequate safeguards to protect vulnerable individuals. The identification and mitigation of these vulnerabilities are crucial for the ethical implementation of MAID. Rigorous evaluation processes and support systems for patients are essential to prevent potential abuse and ensure that MAID is applied responsibly.
Ethical Arguments for and Against MAID
| Argument | Perspective | Summary |
|---|---|---|
| Autonomy and Self-Determination | Pro-MAID | Individuals should have the right to decide how and when their life ends, especially when facing unbearable suffering. |
| Relief of Suffering | Pro-MAID | MAID provides a compassionate option for individuals experiencing unbearable pain and suffering, ensuring a peaceful death. |
| Sanctity of Life | Anti-MAID | The inherent value of human life should be preserved at all costs, and ending a life, even with consent, is ethically wrong. |
| Potential for Abuse | Anti-MAID | Concerns exist about potential coercion, undue influence, or exploitation of vulnerable individuals within the MAID process. |
| Impact on Healthcare Resources | Anti-MAID | Implementing MAID might strain healthcare resources, potentially diverting resources from other critical care areas. |
Support Systems and Care
Navigating the complex decision of Medical Aid in Dying (MAID) requires comprehensive support for patients and their families. This crucial aspect ensures that individuals facing end-of-life decisions receive the necessary care and emotional support throughout the process. Beyond the medical aspects, a robust network of support systems is essential for a smooth and compassionate experience.Understanding the emotional and practical needs of patients considering MAID is paramount.
This includes providing access to a range of services, from palliative care to emotional counseling, to help individuals make informed decisions and navigate the challenging journey ahead. It’s about fostering a supportive environment that allows for open communication and a shared understanding of the patient’s wishes and circumstances.
Palliative Care in the Context of MAID
Palliative care plays a vital role in MAID, providing comprehensive care that focuses on symptom management and improving quality of life for individuals facing serious illness. This includes addressing physical pain, emotional distress, and practical concerns. Palliative care teams work closely with MAID teams to ensure a coordinated approach that addresses all aspects of the patient’s needs, offering comfort and support.
This collaboration is critical in ensuring that patients experience the best possible quality of life until the end.
Emotional Support for Patients and Families
Emotional support is crucial for both the patient and their family during the MAID process. Counseling services, support groups, and individual therapy can help patients and families cope with the emotional burden of the decision. These services aim to provide a safe space for expressing feelings, addressing concerns, and finding ways to navigate the difficult emotions associated with end-of-life choices.
Thinking about death and medical aid in dying is tough, but it’s also important. The political landscape is changing too, with candidates like Biden taking on Trump and promoting a massive infrastructure plan for the next decade, like the one detailed in this article on CNN Break: taking on trump biden promotes infrastructure decade in wisconsin. Ultimately, the decisions we make about end-of-life care are deeply personal, and discussions like these are vital for a healthy society.
Professional counselors can help families understand the patient’s perspective and facilitate open communication.
Community Support Organizations
Numerous community support organizations are dedicated to providing assistance to patients and families considering MAID. These organizations often offer resources, guidance, and a network of support. They provide information on the MAID process, advocate for patient rights, and connect individuals with relevant services. Examples include hospice organizations, palliative care centers, and non-profit organizations specializing in end-of-life care.
These organizations can be invaluable resources for patients and families facing these complex decisions.
Table of Support Services
Historical Context and Evolution
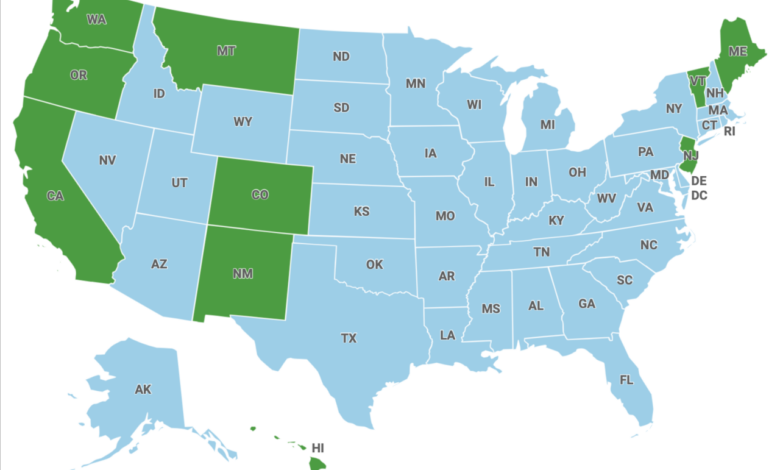
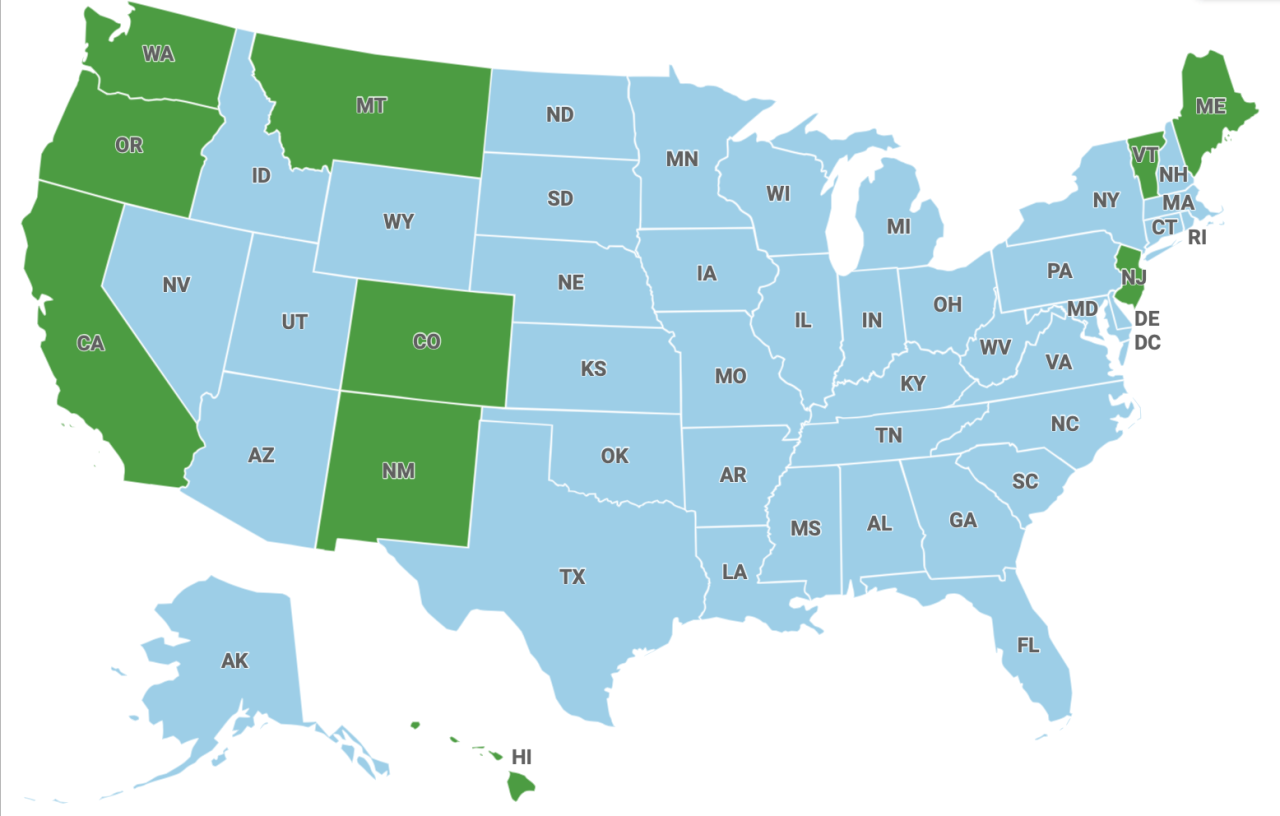
The concept of medical aid in dying (MAID) has roots in a long and evolving debate about individual autonomy, the right to die, and the role of medicine in the face of terminal illness. This exploration delves into the historical journey of MAID, from its earliest philosophical underpinnings to its current legal and societal landscape.The acceptance and implementation of MAID are not uniform across the globe.
Variations in cultural values, religious beliefs, and legal traditions have significantly influenced the development and acceptance of MAID laws. Understanding this historical context provides crucial insight into the current controversies and debates surrounding MAID.
Early Philosophical and Legal Precedents
Philosophical discussions about the right to die have been ongoing for centuries. Ancient Greek philosophers grappled with issues of life, death, and personal freedom, laying groundwork for later discussions on self-determination. Legal precedents, while not directly addressing MAID, have touched upon themes of autonomy and individual rights, paving the way for future legal battles and societal shifts.
Evolution of MAID Laws and Policies
The formalization of MAID laws began in the late 20th century. Early adopters of MAID legislation focused on crafting frameworks for patients with terminal illnesses, prioritizing their autonomy in decision-making. These early laws emphasized stringent criteria for eligibility, ensuring that the practice was reserved for appropriate circumstances.
Cultural and Societal Factors Influencing Acceptance
The acceptance of MAID is deeply intertwined with cultural and societal values. In societies where individual autonomy and personal dignity are highly valued, MAID is more likely to be accepted. Conversely, in societies where religious or ethical considerations regarding life and death are prominent, MAID may face stronger opposition. Public discourse, media coverage, and personal narratives have all played a role in shaping public opinion regarding MAID.
Historical Legal Battles and Public Debates
Numerous legal battles and public debates have shaped the development of MAID. Cases where individuals challenged the legality of denying access to MAID, or where medical professionals questioned their ethical obligations, often became crucial testing grounds for the legal and ethical boundaries of MAID. These conflicts have pushed societal discussions, highlighting the complexities and nuances surrounding MAID. Significant legal challenges often stemmed from differing interpretations of individual rights, medical ethics, and societal values.
Timeline of Key Developments in MAID Legislation and Public Discourse
| Year | Event | Description |
|---|---|---|
| 1970s | Early philosophical discussions | Initial discussions on the right to die emerge in philosophical circles. |
| 1980s | Increased public awareness | Increased media coverage and public discourse on end-of-life care. |
| 1990s | First MAID legislation | Canada became the first country to legalize MAID. |
| 2000s | Expanding legal frameworks | Several countries and states began enacting MAID laws, including various eligibility criteria. |
| 2010s | Ongoing debate and refinement | Public debates and legal challenges continued, leading to revisions and clarifications of existing MAID legislation. |
| 2020s | Global trends | MAID remains a contested issue, with ongoing debates and evolving legal landscapes globally. |
Final Thoughts
In conclusion, death medical aid in dying presents a delicate balance between individual autonomy and societal well-being. This exploration highlights the complexities of end-of-life decision-making, the crucial role of medical professionals and support systems, and the ongoing ethical discussions surrounding this practice. By understanding the multifaceted aspects of MAID, we can foster informed conversations and create a more compassionate and supportive environment for those facing life-altering choices.
Quick FAQs
What are the key distinctions between MAID and physician-assisted suicide (PAS)?
While both involve a medical professional’s role in a patient’s death, MAID often includes the administration of medications by a medical professional, whereas PAS typically involves the patient self-administering the medication prescribed by the physician.
What are some potential vulnerabilities in the MAID process?
Potential vulnerabilities include coercion, undue influence, and inadequate assessment of a patient’s mental capacity. Proper safeguards are essential to ensure truly voluntary choices.
How does the involvement of mental health professionals impact the MAID process?
Mental health professionals play a crucial role in assessing the patient’s psychological well-being and ensuring the decision is made with a clear and sound mind, free from undue influence or coercion.
What is the role of palliative care in MAID?
Palliative care focuses on improving quality of life for those with serious illnesses. It is crucial in MAID to ensure that patients have access to palliative care alongside MAID options, addressing pain and other symptoms.