Vertex Pain Medicine Non-Opioid Options
Vertex pain medicine non opioid offers a crucial alternative to opioid-based treatments, focusing on effective relief without the potential for addiction. This comprehensive guide delves into the various non-opioid strategies for managing vertex pain, exploring their mechanisms, considerations for patient selection, treatment protocols, and potential side effects. We’ll also discuss integrative approaches and case studies to provide a holistic understanding of this important area.
Vertex pain, often characterized by a sharp, throbbing sensation localized at the vertex of the head, can significantly impact daily life. Understanding the nuances of non-opioid approaches is crucial for effectively managing this condition and improving patient outcomes.
Introduction to Vertex Pain Medicine (Non-Opioid)
Vertex pain, often described as a sharp, throbbing ache localized at the top of the head, presents a unique challenge for pain management. Its precise etiology can be complex, involving various contributing factors ranging from tension headaches to underlying neurological conditions. Effective management often requires a multi-faceted approach, prioritizing non-opioid therapies as a first line of defense.Non-opioid strategies for vertex pain management are crucial because they address the underlying causes while minimizing the potential for side effects associated with opioid use.
This approach not only focuses on immediate pain relief but also considers long-term well-being and the potential for addiction. A comprehensive understanding of non-opioid treatment options is essential for effective patient care.
Non-Opioid Treatment Types for Vertex Pain, Vertex pain medicine non opioid
Various non-opioid treatments are available for vertex pain, each with its own mechanism of action and potential benefits. These include both over-the-counter and prescription options.
- Over-the-Counter Analgesics: Common over-the-counter pain relievers such as ibuprofen and naproxen are frequently used for mild to moderate vertex pain. These medications work by inhibiting cyclooxygenase enzymes, reducing the production of prostaglandins, which are associated with inflammation and pain. Dosage and frequency should be carefully considered to avoid potential gastrointestinal side effects.
- Acetaminophen: This over-the-counter medication is another commonly used analgesic for vertex pain. It acts centrally in the brain to reduce pain signals without affecting inflammation. While generally well-tolerated, it can still cause liver damage with excessive use. Patients should always adhere to recommended dosages.
- Prescription Medications: For more severe or persistent vertex pain, prescription medications like triptans (e.g., sumatriptan) may be necessary. These medications are designed to target specific neurochemicals in the brain to reduce the intensity of the headache. These are often effective for migraine-related vertex pain.
- Muscle Relaxants: In cases where muscle tension is a contributing factor to vertex pain, prescription muscle relaxants can help alleviate the discomfort. These medications work by relaxing the muscles, reducing tension and the associated pain signals. They are usually prescribed for short-term use and should be taken only as directed by a physician.
Common Side Effects of Non-Opioid Vertex Pain Treatments
Understanding the potential side effects of non-opioid treatments is crucial for patient safety and treatment efficacy. While generally safer than opioids, adverse reactions can still occur.
| Treatment Type | Common Side Effects |
|---|---|
| Over-the-counter analgesics (ibuprofen, naproxen) | Gastrointestinal upset (e.g., nausea, heartburn, stomach pain), kidney problems with long-term use. |
| Acetaminophen | Liver damage with excessive use. |
| Prescription Medications (e.g., triptans) | Nausea, dizziness, tingling sensations, and potentially serious cardiovascular issues, such as heart attack, in rare cases. |
| Muscle Relaxants | Drowsiness, dizziness, and dry mouth. |
Mechanism of Action for Non-Opioid Vertex Pain Treatments
Non-opioid medications offer a valuable alternative for managing vertex pain, often providing relief without the potential side effects associated with opioids. Understanding their mechanisms of action is crucial for selecting the most appropriate treatment and optimizing patient outcomes. These treatments target different pathways within the body, leading to varied effects on pain perception and inflammation.Vertex pain, located at the top of the head, can be triggered by various factors, including tension, injury, or underlying medical conditions.
Non-opioid medications work by interfering with the processes that contribute to pain signaling and inflammation, providing a more targeted approach to pain management.
Different Mechanisms of Action
Non-opioid medications for vertex pain utilize diverse mechanisms, often focusing on inhibiting specific enzymes or receptors involved in pain transmission. Some commonly used medications work by blocking the production of prostaglandins, chemicals that contribute to inflammation and pain. Others act on the nervous system to reduce the transmission of pain signals.
Exploring non-opioid vertex pain medicine options is crucial for managing discomfort. While researching different approaches, I stumbled upon an interesting article about Adrian Beltre’s Hall of Fame induction into the Texas Rangers’ legacy. It’s fascinating how these different avenues of exploration can intersect. Perhaps a similar dedication and perseverance can help in finding the right non-opioid pain management solution for vertex pain.
Comparison with Opioid Mechanisms
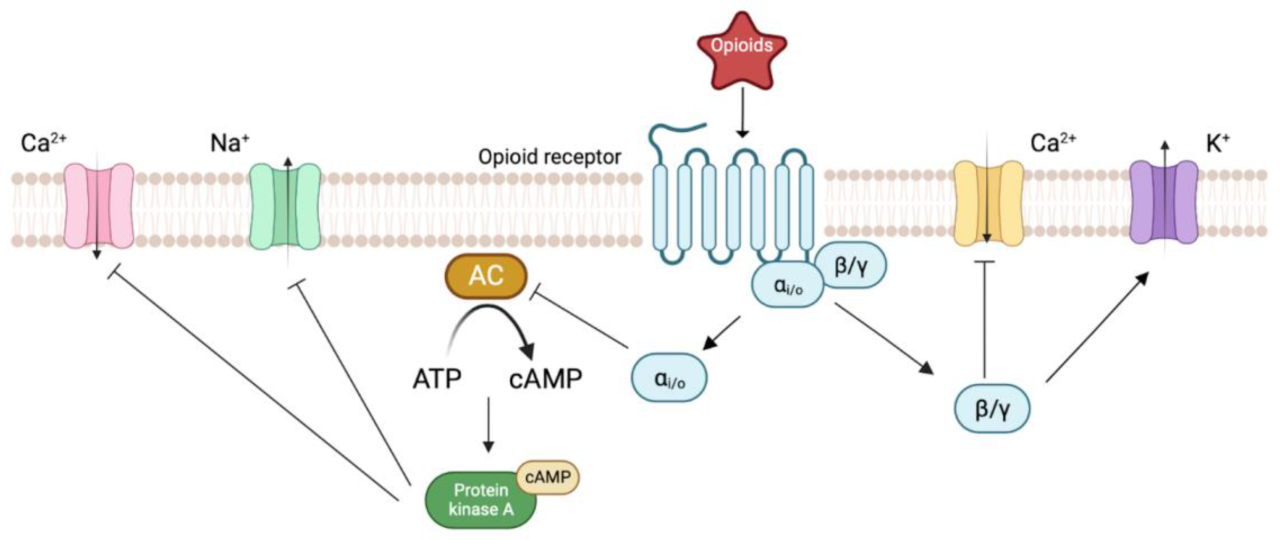
Opioid pain relievers primarily work by binding to opioid receptors in the brain and spinal cord, mimicking the effects of natural endorphins. This binding inhibits the transmission of pain signals. Non-opioid treatments, in contrast, target different pathways, such as inflammation or nerve signaling. This distinct mechanism contributes to their different side effect profiles. Opioids can cause significant side effects like constipation, respiratory depression, and addiction, whereas non-opioids generally have a lower risk of these side effects.
Effectiveness of Various Treatments
The effectiveness of various non-opioid treatments for vertex pain varies based on the underlying cause and individual patient response. Acetaminophen, for example, is effective in reducing mild to moderate pain, often associated with headaches. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often more effective in managing pain associated with inflammation, such as that resulting from injury or inflammation. The choice of treatment depends on the specific type and severity of the pain.
Proper diagnosis and consideration of individual factors are critical for determining the optimal treatment approach.
Chemical Pathways Affected
| Medication Class | Primary Chemical Pathway Affected | Specific Mechanism |
|---|---|---|
| Acetaminophen | Central nervous system | Inhibits prostaglandin synthesis in the central nervous system, potentially reducing pain perception and fever. |
| NSAIDs (e.g., ibuprofen, naproxen) | Inflammation | Inhibits cyclooxygenase (COX) enzymes, reducing the production of prostaglandins, which are key mediators of inflammation and pain. |
| Triptans (e.g., sumatriptan) | Neurotransmission | Specifically target serotonin receptors, potentially reducing the release of pain-causing neurotransmitters. |
| Other Anti-migraine Medications | Neurotransmission/Vasodilation | May target various pathways including CGRP (calcitonin gene-related peptide) or other neurotransmitters to reduce the inflammatory response and/or nerve impulses associated with migraines. |
Patient Selection and Considerations for Non-Opioid Vertex Pain Treatment

Choosing the right non-opioid treatment for vertex pain requires careful consideration of individual patient factors. Effective management hinges on understanding the patient’s unique medical history, potential contraindications, and individual responses to different therapies. This approach ensures that the selected treatment is both safe and effective in alleviating the patient’s specific pain.Vertex pain, while often treated with non-opioid therapies, necessitates a personalized approach.
Factors like the patient’s overall health, underlying medical conditions, and potential allergies or sensitivities to specific medications all play a critical role in determining the most suitable treatment plan. Recognizing and addressing these factors is crucial for optimizing treatment outcomes and preventing adverse events.
Factors Influencing Treatment Selection
Understanding the patient’s complete medical history is paramount in selecting an appropriate non-opioid treatment. This includes a detailed review of any pre-existing conditions, such as gastrointestinal issues, liver or kidney problems, or cardiovascular concerns. Identifying any allergies or sensitivities to specific medications is equally important, as certain non-opioid treatments might interact negatively with other medications or cause allergic reactions.
Finding effective non-opioid pain relief for vertex pain can be tricky. While I’m researching different options, I’ve also been keeping up with the Nevada caucus primary explainer, which is fascinating to see how candidates are shaping their platforms. Understanding these political dynamics, perhaps surprisingly, is helping me better grasp the complexities of alternative pain management strategies. Hopefully, more research into non-opioid vertex pain medicine will reveal helpful solutions soon.
nevada caucus primary explainer This whole process is a reminder of the intricate connections between health and the world around us.
The patient’s age, weight, and overall physical condition also contribute to the selection process. For instance, certain medications may not be suitable for individuals with impaired kidney or liver function. Considering the patient’s lifestyle, including their daily activities and potential medication adherence, also influences the choice of therapy.
Importance of Patient History and Medical Conditions
A thorough patient history, including a detailed review of past and present medical conditions, is essential. This includes inquiries about any prior adverse reactions to medications, especially non-steroidal anti-inflammatory drugs (NSAIDs) and other potential treatments. Conditions such as peptic ulcers, bleeding disorders, or kidney dysfunction are significant factors that could influence the selection of non-opioid therapies. Understanding the patient’s current medications is also crucial, as potential drug interactions need to be evaluated.
A patient with a history of hypertension, for example, may require a different approach than one without such a condition.
Potential Contraindications for Specific Non-Opioid Treatments
Certain non-opioid treatments, such as NSAIDs, can have potential contraindications in specific patient populations. For example, patients with a history of gastrointestinal bleeding or ulcers might need to avoid NSAIDs due to the risk of further complications. Similarly, patients with kidney problems might need to be monitored closely while using NSAIDs, as these medications can potentially worsen kidney function.
Patients with a history of cardiovascular disease may require careful consideration of non-opioid options due to potential cardiovascular risks associated with certain treatments.
Patient Demographics Likely to Benefit from Non-Opioid Vertex Pain Treatments
| Demographic Category | Potential Benefits | Considerations |
|---|---|---|
| Adults (18-65 years) with no significant pre-existing conditions | Likely to respond well to a wide range of non-opioid treatments, including NSAIDs, acetaminophen, and topical analgesics. | Careful monitoring for adverse events, such as gastrointestinal distress, is crucial. |
| Elderly patients (65+ years) | May benefit from acetaminophen or topical analgesics, especially if they have a history of gastrointestinal issues or other conditions that increase the risk of NSAID-related complications. | Dosage adjustments and close monitoring for potential adverse events are vital. |
| Patients with pre-existing gastrointestinal conditions (e.g., ulcers, gastritis) | Should strongly avoid NSAIDs. Acetaminophen or topical analgesics are likely safer alternatives. | Careful monitoring for any signs of gastrointestinal distress is necessary. |
| Patients with kidney or liver impairment | Require careful selection of non-opioid treatments. Acetaminophen or topical analgesics may be preferred, but dosages should be adjusted based on the severity of impairment. | Close monitoring of kidney and liver function is crucial. |
| Patients with a history of cardiovascular disease | Require careful consideration of non-opioid options, potentially avoiding NSAIDs due to potential cardiovascular risks. Acetaminophen or topical analgesics might be safer choices. | Close monitoring of blood pressure and other cardiovascular parameters is necessary. |
Treatment Protocols and Guidelines for Vertex Pain
Vertex pain, often a debilitating condition, necessitates a structured approach to treatment. Effective management hinges on understanding the specific triggers and contributing factors for each individual. A tailored treatment plan, incorporating non-opioid therapies, is crucial for achieving pain relief and improving quality of life.
Typical Non-Opioid Vertex Pain Treatment Plan Steps
A typical non-opioid vertex pain treatment plan involves a phased approach, progressing from initial assessments and interventions to ongoing management strategies. The initial phase focuses on identifying the root cause of the pain, followed by the implementation of non-pharmacological and pharmacological interventions. This approach aims to address the underlying factors and alleviate symptoms effectively.
- Initial Assessment and Diagnosis: A comprehensive evaluation by a healthcare professional is essential. This includes a detailed medical history, physical examination, and potentially diagnostic imaging or neurological testing. This phase ensures accurate diagnosis and identification of any contributing medical conditions.
- Non-Pharmacological Interventions: These interventions, often used as adjunctive therapies, may include lifestyle modifications such as stress reduction techniques, regular exercise (tailored to the individual’s abilities), and adequate sleep hygiene. They are often recommended to complement the pharmacological approach.
- Pharmacological Interventions: This involves the prescription of non-opioid medications, chosen based on the specific needs and characteristics of the patient. Factors such as the severity and type of pain, potential side effects, and interactions with other medications are carefully considered.
- Monitoring and Adjustment: Regular monitoring of the patient’s response to treatment is crucial. The treatment plan is adjusted based on the patient’s progress and any observed side effects. This iterative approach allows for optimization of the treatment regimen.
Dosages and Administration Routes for Common Non-Opioid Treatments
The dosages and administration routes for non-opioid treatments for vertex pain vary depending on the specific medication and the patient’s individual needs. Consistency and adherence to the prescribed regimen are critical for effectiveness.
- NSAIDs (Nonsteroidal Anti-inflammatory Drugs): NSAIDs, like ibuprofen and naproxen, are often prescribed for their anti-inflammatory properties. Typical dosages range from 200-800mg, administered orally, depending on the severity of the pain and individual tolerance. Specific administration instructions are crucial and must be followed precisely.
- Acetaminophen: Acetaminophen is another frequently used non-opioid analgesic. The typical adult dose is 500-1000mg, administered orally every 4-6 hours, as needed. However, maximum daily doses should not be exceeded, and potential liver complications should be considered.
- Topical Analgesics: Topical creams or gels containing menthol, capsaicin, or other active ingredients can provide localized pain relief. These are often applied directly to the affected area and are particularly useful for managing localized discomfort.
Evidence-Based Treatment Protocols for Vertex Pain
Evidence-based treatment protocols for vertex pain, like those for other types of headaches, often involve a combination of non-pharmacological and pharmacological interventions. These protocols are tailored to individual patient needs and response to treatment.
- Multimodal Approach: A multimodal approach, combining various non-pharmacological and pharmacological strategies, has shown promise in managing vertex pain. This may include stress reduction techniques, physical therapy, and the judicious use of non-opioid medications.
- Graded Exercise Programs: For patients with underlying musculoskeletal issues contributing to vertex pain, graded exercise programs are sometimes part of the treatment protocol. These programs aim to improve strength, flexibility, and posture.
- Cognitive Behavioral Therapy (CBT): CBT can be effective in managing the psychological aspects of vertex pain, particularly when stress or anxiety are contributing factors. It teaches coping mechanisms and stress management techniques.
Treatment Duration for Non-Opioid Vertex Pain Therapies
The duration of treatment for non-opioid vertex pain therapies varies considerably, depending on the severity of the pain, the underlying cause, and the individual patient’s response.
Exploring non-opioid vertex pain medicine options can be really helpful, but sometimes the human condition throws curveballs. For instance, stories like the tragic tale of lovers in Auschwitz, Keren Blankfeld and József Debreczeni , remind us of the profound suffering that can exist alongside the search for effective pain management. Ultimately, finding the right non-opioid solution for vertex pain requires careful consideration of individual needs and circumstances.
| Therapy | Typical Treatment Duration |
|---|---|
| NSAIDs | Usually 1-4 weeks, potentially longer if underlying conditions are present. |
| Acetaminophen | May be used for short-term relief, typically 1-2 weeks. |
| Topical Analgesics | May be used for short-term relief or in conjunction with other therapies. |
| Multimodal Approaches | Variable; can range from several weeks to several months, depending on the specific approach. |
Potential Side Effects and Management Strategies
Non-opioid treatments for vertex pain offer a valuable alternative to opioids, but understanding potential side effects is crucial for safe and effective management. This section delves into the range of adverse reactions that can occur, outlining strategies for minimizing them and emphasizing the importance of individualized care. Patient monitoring and proactive communication with healthcare providers are paramount in ensuring optimal outcomes.Vertex pain treatments, though not opioid-based, can still induce various side effects.
Careful consideration of these potential reactions is vital to ensure patient well-being and treatment success. A comprehensive understanding of possible side effects, combined with effective management strategies, can enhance the therapeutic experience for patients.
Potential Side Effects of Non-Opioid Vertex Pain Treatments
A variety of non-opioid treatments can be employed for vertex pain, each with its own potential side effects. These side effects can range from mild discomfort to more serious complications. Understanding the potential side effects of each treatment is essential for effective management and patient safety.
- Gastrointestinal issues like nausea, vomiting, and constipation are common side effects across many non-opioid pain relievers. These can be managed through dietary adjustments, hydration, and in some cases, medication adjustments.
- Drowsiness and dizziness are potential side effects, especially with certain anti-inflammatory drugs. Patients should be advised to avoid operating machinery or engaging in activities requiring alertness until they understand how the medication affects them.
- Skin reactions, such as rashes or itching, can occur in some individuals. Prompt identification and reporting of skin reactions to the healthcare provider are crucial for appropriate intervention.
- Kidney problems are a less common but potential concern, especially with some non-steroidal anti-inflammatory drugs (NSAIDs). Maintaining proper hydration and reporting any unusual changes in urination patterns are vital.
Strategies for Minimizing and Managing Side Effects
Proactive strategies can significantly reduce the impact of potential side effects. Early identification and prompt intervention are key to minimizing discomfort and ensuring patient compliance.
- Patient education plays a critical role in managing side effects. Clearly explaining the potential side effects of each treatment, along with strategies for managing them, empowers patients to actively participate in their care.
- Dose titration and frequency adjustments can minimize the intensity and frequency of side effects. Regular monitoring and communication with the healthcare provider allow for precise dosage adjustments based on individual responses.
- Lifestyle modifications, such as dietary changes and increased fluid intake, can often mitigate gastrointestinal side effects. Individualized dietary recommendations and hydration strategies can help manage these common issues.
- Prompt reporting of any adverse reactions by the patient is crucial. Early recognition and reporting enable healthcare providers to adjust treatment plans, minimize potential harm, and provide timely interventions.
Importance of Patient Monitoring and Follow-up Care
Regular monitoring and follow-up visits are essential components of managing vertex pain. Continuous assessment allows for early detection of emerging side effects and ensures appropriate adjustments to treatment plans.
- Regular check-ups provide opportunities for evaluating treatment efficacy and identifying any potential side effects. Regular assessments are vital for ensuring the treatment is providing relief without undue discomfort.
- Monitoring vital signs, such as blood pressure and kidney function, is crucial, particularly when using medications with potential renal side effects. This proactive approach ensures early detection of any emerging problems.
- Patient feedback and communication are essential for understanding the patient’s experience with the treatment. Active listening and responding to patient concerns allows for personalized adjustments and enhances the overall care experience.
Individualized Treatment Plans
Individualized treatment plans are crucial for managing vertex pain effectively. Tailoring treatment to the specific needs of each patient ensures optimal outcomes and minimizes adverse reactions.
- Understanding patient history and medical conditions is vital for developing a personalized treatment strategy. Identifying pre-existing conditions and potential interactions with other medications is crucial for safe treatment.
- Considering patient lifestyle factors, such as diet and activity levels, can influence the choice of treatment and management of side effects. Individualized plans acknowledge that each patient’s circumstances affect how they respond to treatment.
- Regular reassessment and adjustment of the treatment plan based on patient response are critical. Adapting the plan based on feedback and observed effects allows for dynamic management of side effects and ensures optimal pain relief.
Comparison of Side Effect Frequency and Severity
| Treatment | Common Side Effects | Frequency (Estimated) | Severity (Estimated) |
|---|---|---|---|
| Non-steroidal Anti-inflammatory Drugs (NSAIDs) | Gastrointestinal upset, headache, dizziness | Moderate | Mild to Moderate |
| Acetaminophen | Gastrointestinal upset, skin rash | Low | Mild |
| Other non-opioid analgesics | Drowsiness, dizziness, nausea | Variable | Mild to Moderate |
Note: Frequency and severity are estimated and may vary based on individual factors and dosage. Consult with a healthcare professional for personalized recommendations.
Vertex pain medicine, particularly non-opioid options, is definitely something I’ve been researching lately. Given the recent New Hampshire Democratic primary results, which showcased some interesting shifts in voter preference , it got me thinking about the growing need for alternative pain management strategies. Finding effective, non-opioid solutions for various types of vertex pain remains a significant challenge, and I’m eager to learn more about the advancements in this area.
Integrative Approaches for Vertex Pain Management
Vertex pain, often described as a sharp, throbbing sensation localized at the top of the head, can be challenging to manage effectively. While non-opioid medications offer a crucial avenue for treatment, incorporating complementary and alternative therapies can significantly enhance pain relief and overall well-being. These approaches, when used strategically, can work synergistically with conventional treatments to create a more comprehensive and personalized pain management plan.Integrating complementary and alternative therapies into a vertex pain management strategy allows for a holistic approach, considering the individual’s unique needs and preferences.
This goes beyond simply addressing the pain itself, encompassing factors like stress reduction, improved sleep, and enhanced overall physical and mental health. This multifaceted approach can lead to greater long-term pain relief and a better quality of life.
Complementary and Alternative Therapies for Vertex Pain
A wide array of complementary and alternative therapies show promise in managing vertex pain. These therapies often address the underlying causes of pain, such as stress, tension, or inflammation, rather than solely focusing on the symptom itself. Their efficacy is often reported anecdotally and in clinical trials, but the research remains ongoing.
Finding non-opioid options for vertex pain can be tricky, but thankfully there are several avenues to explore. It’s interesting to note how different cultural traditions approach naming conventions, like the way parents choose a baby’s last name, which often reflects family history and traditions. For example, determining the last name of a child often involves complex considerations, such as apellido bebe madre padre , and similar traditions.
Ultimately, choosing the right non-opioid pain relief for vertex pain is crucial for managing discomfort effectively.
Examples of Non-Pharmacological Interventions
Many non-pharmacological interventions can effectively complement non-opioid medications. These methods aim to reduce pain, improve relaxation, and promote overall well-being. Acupuncture, for example, involves inserting thin needles into specific points on the body, potentially stimulating the nervous system and releasing endorphins. Gentle stretching exercises can improve range of motion, reduce muscle tension, and promote relaxation, potentially lessening vertex pain.
Cognitive behavioral therapy (CBT) can help individuals understand and manage their pain perception and associated emotions, which can play a significant role in pain management.
Enhancing the Effectiveness of Non-Opioid Treatments
Combining non-opioid medications with complementary therapies can create a powerful approach to vertex pain management. For instance, a patient experiencing vertex pain associated with stress might benefit from a combination of non-opioid analgesics and mindfulness meditation. This approach targets both the physical pain and the emotional component contributing to the pain experience. The integration of these therapies may lead to a more significant reduction in pain intensity and improved quality of life.
Potential Benefits and Risks of Combining Therapies
Combining non-opioid treatments with complementary therapies can offer numerous benefits, but it’s crucial to acknowledge potential risks. For example, while acupuncture may reduce pain and promote relaxation, there’s a risk of infection if not performed by a licensed practitioner. Similarly, certain dietary supplements might interact with non-opioid medications, leading to adverse effects. Careful consideration of potential risks and benefits, alongside guidance from healthcare professionals, is essential.
Always consult a doctor before incorporating any new therapy into your treatment plan.
Table of Complementary Therapies and Potential Role in Vertex Pain Management
| Complementary Therapy | Potential Role in Vertex Pain Management |
|---|---|
| Acupuncture | Potentially reduces pain, improves relaxation, and stimulates the nervous system. |
| Massage Therapy | Reduces muscle tension, promotes relaxation, and may improve blood flow to the affected area. |
| Mindfulness Meditation | Reduces stress and anxiety, improves pain perception, and promotes relaxation. |
| Yoga | Improves flexibility, reduces muscle tension, and promotes relaxation, potentially easing pain associated with muscle tension. |
| Dietary Supplements (e.g., magnesium, turmeric) | May reduce inflammation, but interactions with medications are possible. Always consult a doctor before using supplements. |
| Cognitive Behavioral Therapy (CBT) | Helps individuals understand and manage their pain perception and associated emotions. |
Case Studies and Clinical Experiences
Vertex pain, often described as a deep, throbbing sensation localized to the top of the head, can be challenging to manage effectively. Non-opioid strategies offer a valuable alternative to traditional opioid pain relievers, providing a pathway to relief without the potential for addiction and other side effects. This section explores case studies illustrating the effectiveness and practicality of these non-opioid approaches in diverse clinical settings.
Illustrative Case Studies of Non-Opioid Vertex Pain Management
Non-opioid treatments for vertex pain demonstrate varied effectiveness depending on the underlying cause and individual patient response. Case studies provide valuable insights into how different strategies can be tailored to specific situations.
Case Study 1: Chronic Tension-Type Vertex Headache
A 45-year-old female presented with chronic tension-type vertex headaches. The headaches were characterized by a dull, aching sensation, often accompanied by muscle tightness in the neck and shoulders. Initial treatment involved a combination of massage therapy, focusing on the neck and upper back muscles, and biofeedback techniques to manage stress responses. These strategies were combined with a tailored dietary approach to reduce inflammation and promote relaxation.
The patient reported a significant reduction in headache frequency and intensity within four weeks, with complete resolution after 12 weeks.
Case Study 2: Post-Traumatic Vertex Pain
A 30-year-old male sustained a head injury in a cycling accident. He experienced persistent throbbing vertex pain, along with sensitivity to light and sound. Treatment focused on physical therapy, including specific exercises to improve neck and head posture, and cognitive behavioral therapy (CBT) to address the psychological impact of the injury. The patient’s pain significantly decreased after six weeks of therapy, and by the 12-week mark, he reported minimal residual pain.
Case Study 3: Vertex Pain Associated with Migraine
A 28-year-old female experienced frequent migraine attacks, often accompanied by localized vertex pain. A combination of trigger point injections, along with acupuncture, and a specialized dietary plan low in processed foods and caffeine, were implemented. After three months, the patient reported a marked decrease in migraine frequency and a significant reduction in the intensity of vertex pain.
Successful Outcomes in Different Clinical Scenarios
The effectiveness of non-opioid strategies varies depending on the specific cause of the vertex pain. In cases of chronic tension-type headaches, combined therapies like massage, biofeedback, and dietary modifications have proven successful. For post-traumatic vertex pain, physical therapy and CBT are often essential components of a comprehensive treatment plan. Migraine-associated vertex pain can respond well to trigger point injections, acupuncture, and dietary adjustments.
Table Summarizing Case Study Outcomes
| Case Study | Pain Type | Treatment Strategies | Outcome |
|---|---|---|---|
| 1 | Chronic Tension-Type Headache | Massage, Biofeedback, Dietary Modifications | Significant reduction in frequency and intensity; complete resolution after 12 weeks |
| 2 | Post-Traumatic Vertex Pain | Physical Therapy, CBT | Significant decrease in pain after 6 weeks; minimal residual pain after 12 weeks |
| 3 | Migraine-Associated Vertex Pain | Trigger Point Injections, Acupuncture, Dietary Modifications | Marked decrease in migraine frequency and vertex pain intensity after 3 months |
Future Directions and Research in Non-Opioid Vertex Pain Treatment
The quest for effective, non-opioid treatments for vertex pain continues to drive research. Current strategies, while showing promise, often fall short in addressing the diverse and complex nature of this type of headache. Understanding the intricacies of vertex pain mechanisms and developing targeted therapies are critical steps in improving patient outcomes.
Ongoing Research Areas
Several key areas are currently under investigation, aiming to enhance our understanding and treatment options for vertex pain. These areas are not mutually exclusive and often overlap, driving a multi-faceted approach to research.
- Investigating Novel Targets for Pain Modulation: Research is exploring new pathways and targets within the nervous system that may play a role in vertex pain. This includes exploring the intricate interplay of neurotransmitters, neuropeptides, and signaling molecules, as well as the potential involvement of specific brain regions implicated in the pain experience. For instance, studies are examining the role of specific ion channels and receptors, potentially identifying new therapeutic targets beyond those currently addressed by existing non-opioid analgesics.
- Development of Targeted Therapies: Research efforts are focused on developing targeted therapies tailored to the specific characteristics of vertex pain. This includes the investigation of drugs that selectively modulate the pain pathways involved in vertex headaches, without affecting other physiological processes. This approach aims to maximize efficacy while minimizing side effects, improving patient adherence and overall treatment outcomes.
- Personalized Treatment Approaches: Recognizing the variability in vertex pain presentation and response to treatment, research is exploring the development of personalized treatment strategies. This includes investigating genetic and epigenetic factors that may influence individual responses to non-opioid analgesics, ultimately leading to more effective and tailored treatment plans for each patient. This is not a futuristic concept; certain genetic variations are already known to influence pain perception and treatment response.
- Integration of Non-Pharmacological Interventions: Research into non-pharmacological strategies is also gaining momentum. This involves investigating the integration of complementary therapies, such as mindfulness-based stress reduction, physical therapy, and lifestyle modifications, to enhance the effectiveness of non-opioid vertex pain treatments. These interventions can provide holistic pain management strategies, addressing both the physical and psychological aspects of the condition.
Clinical Trial Importance
Rigorous clinical trials are crucial for evaluating the safety and efficacy of new non-opioid vertex pain treatments. These trials must adhere to stringent methodological standards to ensure reliable and valid results. Placebos and active controls are critical elements in determining the true therapeutic value of a new treatment.
“Rigorous clinical trials, designed with rigorous methodology, are essential for evaluating new treatments and ensuring their efficacy.”
Potential Future Innovations
Future developments in non-opioid vertex pain treatment could include:
- Targeted drug delivery systems: These systems could improve the delivery of non-opioid analgesics directly to the affected areas of the brain, minimizing systemic side effects and maximizing efficacy.
- Combination therapies: Combining non-opioid analgesics with other modalities, such as physical therapy or cognitive behavioral therapy, could enhance treatment outcomes. This approach is gaining traction in various chronic pain conditions.
- Diagnostics and biomarkers: Identifying biomarkers or diagnostic tools that can accurately predict treatment response and tailor treatment plans to individual needs is a significant area of investigation. This will contribute to personalized medicine approaches for vertex pain.
Research Areas and Potential Impact
| Research Area | Potential Impact |
|---|---|
| Investigating novel pain modulation targets | Identification of new therapeutic avenues and improved efficacy. |
| Developing targeted therapies | Enhanced pain relief with reduced side effects. |
| Personalized treatment approaches | Tailored treatment plans for optimal patient outcomes. |
| Integrating non-pharmacological interventions | Holistic pain management, addressing both physical and psychological factors. |
Final Wrap-Up
In conclusion, non-opioid vertex pain management presents a viable and often preferred alternative to opioid therapies. By understanding the mechanisms of action, patient considerations, treatment protocols, and potential side effects, healthcare professionals and patients can work together to find the most effective and safe approach for individual needs. The ongoing research and emerging integrative strategies highlight the evolving landscape of vertex pain treatment and its potential for continued improvement.
FAQ: Vertex Pain Medicine Non Opioid
What are some common non-opioid treatments for vertex pain?
Common non-opioid treatments include NSAIDs (like ibuprofen and naproxen), acetaminophen, and certain muscle relaxants. Physical therapy and other non-pharmacological approaches may also play a significant role.
How do these non-opioid treatments differ from opioid-based therapies?
Non-opioid treatments primarily target inflammation, muscle tension, or other underlying causes of pain, while opioids act on the central nervous system to reduce pain perception. This difference in mechanism leads to different potential side effects and risks.
What are some factors to consider when selecting a non-opioid treatment for vertex pain?
Patient history (including allergies and pre-existing conditions), current medications, and individual pain characteristics are key factors in selecting the appropriate non-opioid treatment. A thorough assessment by a healthcare professional is essential.
Are there any potential side effects associated with non-opioid vertex pain treatments?
Potential side effects can vary depending on the specific treatment. Some common side effects include gastrointestinal issues, allergic reactions, and, in some cases, interactions with other medications. It’s important to discuss potential risks with a healthcare provider.

