Mild Cognitive Impairment Treatment A Comprehensive Guide
Mild cognitive impairment treatment is a multifaceted approach that aims to address the unique challenges presented by this condition. It encompasses a range of strategies, from lifestyle modifications to pharmacological interventions, all designed to improve cognitive function and quality of life. This guide delves into the intricacies of diagnosing and managing MCI, exploring both the scientific basis and practical implications of various treatment approaches.
Understanding the different types of MCI, from amnestic to non-amnestic, is crucial for tailoring treatment plans. This article will also detail the diagnostic process, highlighting the role of neuropsychological testing and comparing various diagnostic criteria. Furthermore, we’ll examine the importance of lifestyle factors in preventing MCI, including diet, exercise, and social engagement. Supporting caregivers and exploring the current research in MCI treatment will also be addressed.
Introduction to Mild Cognitive Impairment (MCI)
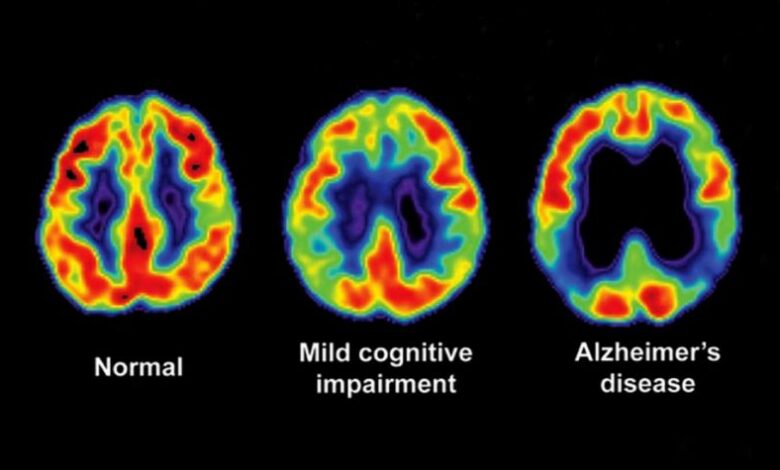
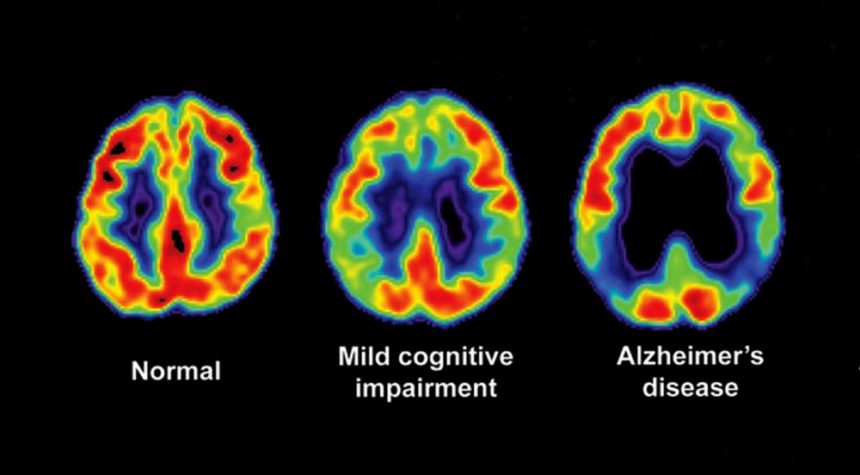
Mild cognitive impairment (MCI) represents a transitional stage between normal age-related cognitive decline and the more serious symptoms of dementia. It’s characterized by a noticeable decline in cognitive function that is greater than expected for a person’s age and education level, but not severe enough to interfere significantly with daily activities. This subtle yet persistent decline can affect various cognitive domains, potentially foreshadowing future cognitive decline in some individuals.MCI is not a disease itself, but rather a syndrome that often precedes the development of dementia, particularly Alzheimer’s disease.
Understanding the characteristics, symptoms, and types of MCI is crucial for early detection and intervention, enabling individuals to proactively address potential cognitive challenges and maintain their independence for as long as possible.
Defining Mild Cognitive Impairment (MCI)
Mild cognitive impairment (MCI) is a condition characterized by a noticeable decline in cognitive function beyond what’s typical for a person’s age and education level. This decline is significant enough to be noticed by the individual or others, but not severe enough to interfere substantially with daily activities. Crucially, it doesn’t meet the diagnostic criteria for dementia.
Key Characteristics and Symptoms of MCI
Individuals with MCI often experience difficulties in one or more cognitive domains, such as memory, language, attention, executive function, or visuospatial skills. Common symptoms may include:
- Problems with remembering recent events or conversations.
- Difficulty finding the right words or following complex instructions.
- Reduced ability to plan or organize tasks.
- Getting lost in familiar places.
- Difficulty with judgment or decision-making.
It’s important to remember that these symptoms can vary significantly in severity and frequency among individuals with MCI. Furthermore, the specific symptoms often depend on the type of MCI a person has.
Differentiating MCI from Normal Age-Related Cognitive Decline
While age-related cognitive changes are normal, MCI represents a more substantial decline. Distinguishing between the two can be challenging, requiring careful evaluation by a healthcare professional. Significant differences include the impact on daily life and the level of impairment. Individuals with MCI may experience noticeable issues in their daily activities that affect their quality of life.
Types of Mild Cognitive Impairment (MCI)
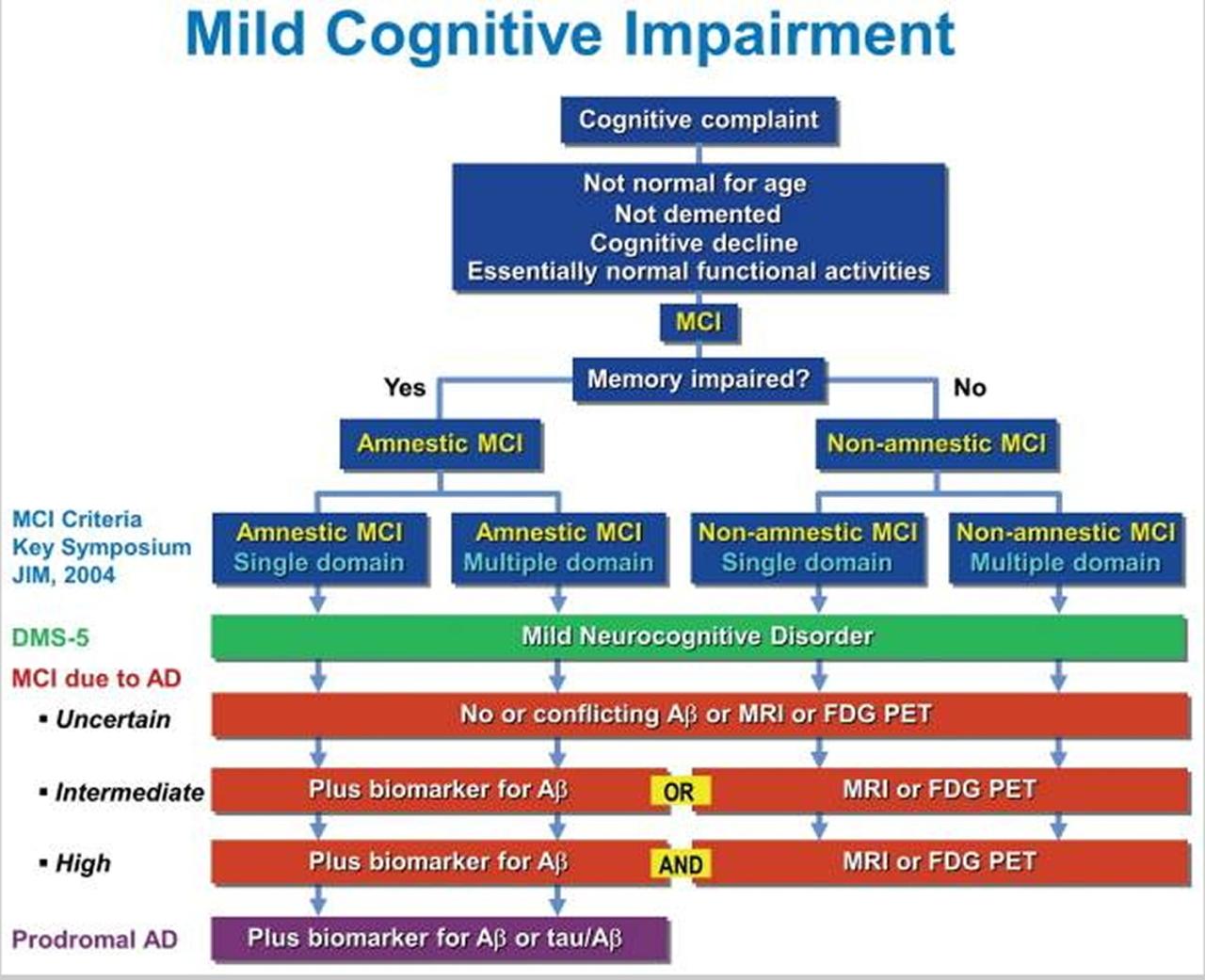
MCI is categorized into different subtypes based on the specific cognitive domains affected. The most common types are:
- Amnestic MCI: Characterized by memory problems as the primary symptom. This is the most common type of MCI and is often associated with an increased risk of developing Alzheimer’s disease.
- Non-amnestic MCI: Involves problems in other cognitive domains, such as language, attention, executive function, or visuospatial skills, without significant memory impairment. These subtypes also pose a risk of future cognitive decline.
Symptom Profiles Across MCI Types
The table below provides a general overview of symptom profiles across different MCI types. Note that these are general trends and individual experiences can vary considerably.
| Symptom | Frequency | Severity |
|---|---|---|
| Amnestic MCI (Memory problems) |
Frequently | Moderate to Severe |
| Non-amnestic MCI (Language) (Language difficulties) |
Occasional to Frequent | Mild to Moderate |
| Non-amnestic MCI (Executive function) (Planning and organizing difficulties) |
Occasional to Frequent | Mild to Moderate |
| Non-amnestic MCI (Visuospatial) (Problems with spatial awareness) |
Occasional to Frequent | Mild to Moderate |
Diagnosis and Assessment
Diagnosing mild cognitive impairment (MCI) requires a careful and comprehensive approach, moving beyond simple screening tools to detailed assessments. The process aims to differentiate MCI from normal age-related cognitive decline and other conditions that might mimic MCI symptoms. This involves evaluating various cognitive domains, considering the patient’s medical history, and often comparing results to established norms.A key aspect of MCI diagnosis is the recognition that it exists on a spectrum.
Individuals with MCI experience subtle but measurable cognitive difficulties, which can vary in severity and across different cognitive functions. Consequently, diagnosis hinges on a thorough understanding of the individual’s baseline cognitive abilities and the identification of significant declines compared to those abilities. These declines must also be significant enough to impact daily functioning but not severe enough to meet the criteria for dementia.
Mild cognitive impairment (MCI) treatment is a fascinating area of research, and there are many avenues being explored. Recent studies have shown promising results with non-invasive methods, but some researchers are also looking into more innovative approaches, such as the potential benefits of the Castellucci ring La Monnaie. This ring is designed to stimulate specific neural pathways, and some preliminary data suggests it might have a positive impact on cognitive function.
Ultimately, more research is needed to determine the long-term effectiveness of these methods in treating MCI.
Methods for Diagnosing MCI
Various methods contribute to the accurate diagnosis of MCI. These include detailed interviews with the patient and their caregivers, focusing on their cognitive and functional abilities over time. Neuropsychological testing plays a crucial role in evaluating specific cognitive domains, such as memory, attention, language, and executive functions. These tests provide quantitative data that can be compared to established norms for individuals of similar age, education, and cultural background.
Mild cognitive impairment (MCI) treatment is a complex area, with various approaches and no single “cure-all.” Understanding the demographics of different regions, like the variations in red blue states demographics , could potentially offer insights into how access to care and lifestyle factors might influence MCI prevalence and outcomes. Ultimately, a multifaceted approach, considering individual needs and community resources, is crucial for effective MCI treatment strategies.
Physical and neurological examinations are also important to rule out other potential causes for the observed cognitive difficulties.
Tools and Tests in the Diagnostic Process
Numerous tools and tests are employed in the diagnostic process. Standardized neuropsychological tests, such as the Montreal Cognitive Assessment (MoCA), the Mini-Mental State Examination (MMSE), and the Clock Drawing Test, are frequently used. These tests assess various cognitive domains and provide a quick overview of cognitive function. More comprehensive assessments may involve tasks evaluating specific cognitive abilities like memory encoding and retrieval, processing speed, and visuospatial skills.
The specific tests utilized often depend on the suspected cognitive strengths and weaknesses of the individual being assessed.
Comparison of Assessment Methods
Different assessment methods for MCI offer varying levels of detail and depth. While screening tools like the MoCA and MMSE are useful for initial evaluations and identifying potential concerns, more in-depth neuropsychological testing provides a more comprehensive picture of cognitive strengths and weaknesses. The choice of assessment method should be tailored to the individual patient and the specific clinical context.
For instance, a patient with a strong family history of Alzheimer’s disease might benefit from a more comprehensive assessment to rule out early-stage dementia.
Role of Neuropsychological Testing in MCI Diagnosis
Neuropsychological testing is indispensable in the diagnosis of MCI. These tests are designed to assess various cognitive functions, providing quantitative data on performance in areas like memory, attention, language, and executive functions. The results are then compared to normative data, allowing clinicians to identify any significant discrepancies that may suggest MCI. Importantly, the test results are considered in conjunction with the patient’s medical history, caregiver reports, and other clinical information to form a complete picture of the individual’s cognitive profile.
Diagnostic Criteria Across Different Systems
| Diagnostic System | Key Criteria for MCI |
|---|---|
| DSM-5 | Significant cognitive decline from a previous level of performance, but not interfering with daily activities. Cognitive deficits in one or more cognitive domains. Not meeting criteria for dementia. |
| ICD-11 | Presence of cognitive complaints or concerns from the individual or their informants. Objective evidence of cognitive impairment in one or more cognitive domains. No impairment in daily activities. |
This table provides a concise overview of the key criteria for MCI across different diagnostic systems. Note that these criteria may overlap, but differences in emphasis and the specific cognitive domains assessed may exist. It’s crucial for clinicians to consult the relevant diagnostic guidelines for the most accurate and comprehensive assessment.
Treatment Approaches
Mild Cognitive Impairment (MCI) doesn’t have a cure, but various strategies can help manage symptoms and potentially slow its progression. Treatment focuses on improving cognitive function, promoting overall well-being, and enhancing quality of life for individuals with MCI. This approach encompasses both non-pharmacological interventions and lifestyle modifications.Non-pharmacological interventions, particularly cognitive training and lifestyle adjustments, play a crucial role in managing MCI.
Evidence suggests that consistent engagement in these strategies can lead to noticeable improvements in cognitive performance and daily functioning.
Non-Pharmacological Interventions
These interventions aim to stimulate and maintain cognitive function without the use of medication. They are often recommended in conjunction with lifestyle modifications for a comprehensive approach to managing MCI.
- Cognitive Training Programs: These structured programs provide exercises designed to improve specific cognitive skills, such as memory, attention, and processing speed. They often involve repetition and gradual progression to challenge and strengthen cognitive abilities. A variety of formats, from computerized tasks to group-based activities, are available.
- Lifestyle Modifications: Adopting healthy habits can significantly impact cognitive function. Maintaining a balanced diet, regular exercise, sufficient sleep, and stress management are key aspects of this approach. For instance, studies have shown that individuals with MCI who engage in regular physical activity often experience improved cognitive performance.
- Social Support: Maintaining a strong social network and engaging in meaningful social interactions can be beneficial for individuals with MCI. Socialization can provide cognitive stimulation, emotional support, and a sense of belonging. This support network can be a family, friends, or support groups. Strong social connections can buffer the effects of cognitive decline.
Cognitive Training Programs
Cognitive training programs are designed to enhance specific cognitive functions. They can be customized to target areas where an individual is experiencing difficulty.
- Computerized Cognitive Training: Software programs offer a variety of interactive exercises targeting memory, attention, and problem-solving skills. They often provide personalized feedback and adaptive difficulty levels. Examples include programs focused on memory recall, attention span, and reaction time. One example is Cogmed, which is a widely used program for working memory training.
- Memory Training: This involves strategies to improve memory retention and recall. Techniques such as mnemonics, spaced repetition, and memory palace methods are often employed. Memory aids, like calendars and to-do lists, can also be incorporated. The key is finding strategies that resonate with the individual’s learning style.
- Attention Training: These programs focus on improving concentration and sustained attention. Activities might include tasks requiring focused attention, filtering distractions, or tasks that require vigilance. Examples include tasks that require sustained attention or visual search tasks.
- Problem-Solving Training: This involves exercises that challenge logical reasoning and decision-making abilities. They can include puzzles, brain teasers, and problem-solving scenarios. The goal is to enhance critical thinking and problem-solving skills.
Lifestyle Modifications for MCI
These modifications aim to reduce risk factors and promote overall health, contributing to better cognitive function. A balanced approach is key to maximizing benefits.
- Healthy Diet: A diet rich in fruits, vegetables, and whole grains, with limited processed foods, sugary drinks, and saturated fats, is often recommended. Studies suggest a link between a Mediterranean-style diet and improved cognitive function.
- Regular Exercise: Physical activity is crucial for overall health and may contribute to better cognitive function. Aerobic exercise, strength training, and flexibility exercises are beneficial.
- Adequate Sleep: Sufficient sleep is essential for cognitive restoration and consolidation. Aim for 7-9 hours of quality sleep per night.
- Stress Management: Chronic stress can negatively impact cognitive function. Practices like mindfulness, meditation, and yoga can help manage stress levels.
Social Support and MCI
Maintaining a strong social network is vital for managing MCI. Social interaction provides cognitive stimulation, emotional support, and a sense of belonging, all contributing to well-being.
- Social Interaction: Engaging in social activities, such as joining clubs, volunteering, or participating in group discussions, can offer significant cognitive benefits. Regular interaction with loved ones can also be important.
- Support Groups: Support groups provide a safe space for individuals with MCI and their families to share experiences, learn coping strategies, and connect with others facing similar challenges. This shared experience fosters a sense of community and mutual understanding.
Comparing Cognitive Training Exercises
| Exercise Type | Description | Potential Benefits |
|---|---|---|
| Computerized Cognitive Training | Interactive software exercises targeting memory, attention, and problem-solving. | Personalized feedback, adaptive difficulty, improved cognitive skills. |
| Memory Training | Strategies to improve memory retention and recall, like mnemonics and memory aids. | Enhanced memory capacity, improved recall, better organization of information. |
| Attention Training | Activities focusing on concentration and sustained attention. | Improved focus, reduced distractions, enhanced multitasking abilities. |
| Problem-Solving Training | Exercises challenging logical reasoning and decision-making. | Improved critical thinking, enhanced problem-solving skills, better decision-making. |
Pharmacological Interventions
Currently, there’s no cure for mild cognitive impairment (MCI), but pharmacological interventions aim to slow its progression and potentially improve cognitive function. While no medication definitively halts or reverses MCI, some medications show promise in managing specific symptoms or underlying conditions that might contribute to cognitive decline. This section delves into the existing medications used for MCI management, their rationale, potential benefits, and risks, along with ongoing research.Pharmacological interventions in MCI treatment primarily focus on addressing potential underlying causes, such as vascular issues, neurotransmitter imbalances, or inflammation.
The rationale is to target these factors to potentially slow cognitive decline and improve overall quality of life. While individual responses vary, the hope is that these interventions can provide a tangible benefit in managing the symptoms and the overall progression of the condition.
Current Medications Used for MCI
Several medications are being explored for potential use in MCI management. These include cholinesterase inhibitors, memantine, and other medications targeting specific contributing factors. Understanding their mechanisms of action, potential benefits, and risks is crucial for informed decision-making.
Rationale for Using Medications in MCI Management
The rationale behind using these medications in MCI management is rooted in the potential underlying causes of cognitive decline. Cholinesterase inhibitors, for example, aim to increase levels of acetylcholine, a neurotransmitter crucial for memory and learning. Memantine, on the other hand, works by modulating glutamate activity, a neurotransmitter implicated in neuronal damage. These interventions aim to mitigate the factors contributing to cognitive decline, even if a complete reversal isn’t achievable.
Potential Benefits and Risks of Each Medication
Cholinesterase inhibitors, such as donepezil and rivastigmine, may improve memory and other cognitive functions in some individuals with MCI. However, potential side effects include nausea, vomiting, diarrhea, and headaches. Memantine, while potentially slowing cognitive decline, might cause dizziness, headache, and constipation. The specific benefits and risks vary from person to person, making careful monitoring and consideration essential.
Ongoing Research on Pharmacological Treatments for MCI
Ongoing research continues to explore the efficacy and safety of various medications in MCI management. Researchers are investigating the use of other medications, such as anti-inflammatory drugs and medications targeting specific vascular factors, in potentially slowing cognitive decline. Clinical trials are evaluating the effectiveness and safety profiles of these treatments.
Comparison of Efficacy and Side Effects of Medications for MCI
| Medication | Mechanism of Action | Potential Benefits | Potential Side Effects | Efficacy Evidence |
|---|---|---|---|---|
| Cholinesterase Inhibitors (e.g., Donepezil, Rivastigmine) | Increase acetylcholine levels | Potential improvement in memory and cognitive function | Nausea, vomiting, diarrhea, headaches | Mixed results, some studies show modest improvement in cognitive function |
| Memantine | Modulates glutamate activity | Potential slowing of cognitive decline | Dizziness, headache, constipation | Some studies show potential slowing of cognitive decline, but results are not conclusive |
| Other Medications (e.g., Anti-inflammatory drugs) | Targeting specific factors | Potential impact on inflammation and vascular issues | Potential side effects dependent on specific drug | Ongoing research to determine efficacy |
Lifestyle Factors and Risk Reduction
Mild Cognitive Impairment (MCI) isn’t an inevitable consequence of aging. Numerous lifestyle factors significantly influence the risk of developing MCI. Adopting healthy habits can play a crucial role in mitigating the risk and potentially slowing its progression. Understanding these factors and implementing positive changes can contribute to maintaining cognitive health throughout life.
Mild cognitive impairment (MCI) treatment is a fascinating area of research, with various approaches being explored. One interesting angle is how potential societal changes might affect MCI outcomes. For example, a recent article on Steve Garvey’s California Senate campaign ( steve garvey california senate ) highlights the importance of accessible information and support systems for older adults.
This ultimately connects back to the ongoing quest for effective MCI treatment strategies.
Impact of Lifestyle Factors on MCI Risk
Lifestyle choices have a profound impact on cognitive health. A combination of factors, including diet, exercise, social engagement, mental stimulation, and stress management, can significantly affect the risk of developing MCI. Studies have consistently shown that individuals who maintain healthy lifestyles tend to have a lower likelihood of developing MCI compared to those with less healthy habits.
Importance of a Healthy Diet in Preventing MCI
A balanced and nutritious diet is fundamental to overall health, including brain health. A diet rich in fruits, vegetables, whole grains, and lean protein, along with healthy fats, can provide the essential nutrients needed for optimal brain function. Conversely, a diet high in processed foods, saturated fats, and added sugars can contribute to inflammation and oxidative stress, potentially increasing the risk of MCI.
For example, studies have linked diets rich in antioxidants, found in berries and leafy greens, to improved cognitive function and a reduced risk of age-related cognitive decline.
Importance of Exercise in Preventing MCI
Regular physical activity is crucial for maintaining cognitive health. Exercise improves blood flow to the brain, promoting the growth of new brain cells and improving overall brain function. This, in turn, can help reduce the risk of developing MCI. Aerobic exercises, such as brisk walking, jogging, or swimming, are particularly beneficial. Even moderate-intensity activities like gardening or taking the stairs can make a difference.
Finding effective treatments for mild cognitive impairment (MCI) is a real challenge. While exploring different avenues, I’ve been strangely captivated by the intricate musicality of Broadway cast albums, particularly the haunting melodies of Sweeney Todd. Listening to the broadway cast albums sweeney todd has unexpectedly sparked some interesting connections in my mind, and I’m hoping these musical explorations might eventually inspire innovative approaches to MCI treatment.
It’s a long shot, but hey, anything is worth a try, right?
For example, research has shown that individuals who engage in regular exercise tend to maintain better cognitive function as they age, demonstrating a direct link between physical activity and brain health.
Role of Social Engagement in MCI Prevention
Maintaining social connections and engagement is vital for cognitive health. Social interaction stimulates the brain, helping to maintain cognitive function and memory. Participating in social activities, such as joining clubs, volunteering, or spending time with loved ones, can contribute to a lower risk of developing MCI. For example, individuals who participate in regular social activities demonstrate better cognitive performance and reduced incidence of cognitive decline.
Role of Mental Stimulation in MCI Prevention
Mental stimulation plays a crucial role in maintaining cognitive function. Activities that challenge the brain, such as learning new skills, reading, playing games, or engaging in puzzles, can help keep the mind sharp. These activities promote neuroplasticity, which is the brain’s ability to adapt and change throughout life. For example, individuals who engage in intellectually stimulating activities, like learning a new language or playing a musical instrument, often experience a slower decline in cognitive function.
Significance of Stress Management Techniques in Reducing MCI Risk
Chronic stress can negatively impact brain health, potentially increasing the risk of MCI. Effective stress management techniques, such as mindfulness, meditation, deep breathing exercises, or yoga, can help regulate stress hormones and promote relaxation. These techniques can contribute to better cognitive function and reduce the risk of developing MCI. For instance, studies have shown that individuals who practice mindfulness or meditation have better cognitive performance and a lower level of stress hormones.
Summary of Lifestyle Recommendations for Reducing MCI Risk
| Activity Type | Recommendations |
|---|---|
| Physical | Regular aerobic exercise (e.g., brisk walking, jogging, swimming); maintaining a healthy weight; strength training; balance exercises. |
| Social | Maintaining active social connections; engaging in social activities; participating in community events; spending time with loved ones. |
| Mental | Learning new skills; reading; playing games; engaging in puzzles; challenging the brain with intellectually stimulating activities. |
| Stress Management | Practicing mindfulness; meditation; deep breathing exercises; yoga; seeking professional help if needed. |
| Diet | Following a balanced diet rich in fruits, vegetables, whole grains, and lean protein; limiting processed foods, saturated fats, and added sugars. |
Supporting Caregivers: Mild Cognitive Impairment Treatment
Caring for someone with mild cognitive impairment (MCI) can be a significant undertaking, impacting the emotional, physical, and financial well-being of caregivers. Navigating the changing needs of a loved one, while also maintaining personal responsibilities, can be challenging and overwhelming. Understanding the unique demands of this role and having access to appropriate support is crucial for both the caregiver and the individual with MCI.The caregiver’s role often involves a complex blend of tasks, including assisting with daily activities, managing medications, providing emotional support, and advocating for their loved one’s needs.
This responsibility can lead to considerable stress and burnout if not managed effectively. This section will explore the challenges faced by caregivers, the importance of support systems, strategies for managing stress, and the necessity of education and awareness.
Challenges Faced by Caregivers
Caregivers of individuals with MCI often experience a wide array of challenges. These challenges encompass emotional burdens, like witnessing the gradual decline in cognitive abilities and the frustration associated with the changes in behavior. The practical demands of caregiving, such as managing appointments, coordinating care, and ensuring safety, can be overwhelming and time-consuming. Financial strain is another significant concern, as caregiving often requires adjustments to work schedules or taking time off from employment.
Furthermore, caregivers may experience social isolation as they dedicate more time to caregiving responsibilities, potentially neglecting other relationships and interests.
Importance of Support Groups and Resources
Support groups provide a crucial platform for caregivers to connect with others who understand their experiences. Sharing stories, strategies, and coping mechanisms fosters a sense of community and reduces feelings of isolation. Access to resources, such as educational materials, information about available services, and practical tips for managing daily tasks, is essential for caregivers to feel empowered and equipped to handle their responsibilities effectively.
Caregivers can find comfort and strength in knowing they are not alone in their journey.
Strategies for Managing Caregiver Stress and Burnout
Managing caregiver stress and burnout requires proactive strategies. These include prioritizing self-care activities, such as exercise, relaxation techniques, and maintaining social connections. Setting realistic expectations and boundaries is crucial, acknowledging the limitations of one’s capacity and seeking support when needed. Learning to delegate tasks, whether to other family members, professional caregivers, or community services, can significantly reduce the burden.
Seeking professional counseling or therapy can provide valuable coping mechanisms and strategies for managing emotional distress.
Recent research on mild cognitive impairment treatment is really promising, focusing on lifestyle changes and targeted therapies. While global events like the ongoing Biden-Israel-Hamas cease fire situation here can understandably take a toll on mental well-being, it’s crucial to remember that consistent cognitive stimulation and a healthy diet are still key to managing and potentially preventing mild cognitive impairment.
Importance of Education and Awareness for Caregivers
Education plays a pivotal role in empowering caregivers. Understanding the progression of MCI, the various treatment options, and the potential challenges can help caregivers make informed decisions and effectively advocate for their loved one. Awareness of available resources, support groups, and community services is essential for accessing the necessary assistance and minimizing stress. Caregivers who are well-informed and supported are better equipped to provide quality care and maintain their own well-being.
Resources and Support Groups for Caregivers of Individuals with MCI
| Resource Type | Description | Contact Information (Example) |
|---|---|---|
| Support Groups | Provide a supportive environment for caregivers to connect with others facing similar challenges. | Alzheimer’s Association, local support groups |
| Online Forums | Offer online platforms for connecting with other caregivers and sharing experiences. | Caregiver support forums on websites like Mayo Clinic, Healthline |
| Local Agencies | Offer practical assistance, counseling, and support services. | Area Agencies on Aging, local senior centers |
| Professional Counseling | Provide individual or group therapy for managing stress and emotional well-being. | Licensed therapists, social workers |
| Educational Materials | Offer information on MCI, treatment options, and resources. | Alzheimer’s Association website, local health department |
Current Research and Future Directions
The journey of understanding and treating mild cognitive impairment (MCI) is a dynamic one, marked by ongoing research and emerging therapies. Researchers are actively exploring various avenues to improve the lives of individuals affected by MCI, focusing on preventing progression to Alzheimer’s disease and enhancing cognitive function. This exploration encompasses a range of strategies, from pharmacological interventions to lifestyle modifications and innovative diagnostic tools.This exciting phase of research promises to lead to a more nuanced understanding of MCI and ultimately, more effective treatment options.
The goal is not only to halt or reverse cognitive decline but also to improve the overall quality of life for individuals experiencing MCI.
Ongoing Research in MCI Treatment, Mild cognitive impairment treatment
A multitude of studies are investigating the efficacy of various interventions for MCI. These studies are designed to assess the impact of specific treatments on cognitive function, daily activities, and the risk of progression to Alzheimer’s disease. Researchers are utilizing advanced neuroimaging techniques and sophisticated cognitive assessments to gather data. This rigorous approach helps to isolate the effects of interventions and to identify potential biomarkers of disease progression.
Emerging Therapies and Approaches
New therapeutic strategies are constantly emerging in the field of MCI treatment. One promising area involves the development of drugs that target specific molecular pathways implicated in the pathogenesis of Alzheimer’s disease, which is often linked to MCI. Researchers are also exploring non-pharmacological interventions, such as cognitive training programs, physical exercise, and nutritional strategies. These approaches aim to improve cognitive reserve and overall well-being.
For example, a recent study showed a significant improvement in memory function in individuals with MCI who engaged in regular aerobic exercise.
Personalized Medicine in MCI Management
The concept of personalized medicine is gaining traction in MCI management. This approach recognizes that individuals with MCI may respond differently to various treatments. By analyzing genetic factors, lifestyle choices, and other individual characteristics, researchers aim to tailor interventions to each patient’s specific needs. This tailored approach may lead to more effective treatments and improved outcomes. For instance, genetic testing might identify individuals who are at higher risk for progression, enabling early intervention and personalized strategies to mitigate that risk.
Importance of Clinical Trials in Advancing MCI Treatment
Clinical trials play a crucial role in evaluating the safety and efficacy of new treatments for MCI. These trials rigorously assess the effects of interventions in a controlled setting, helping to ensure that promising therapies are both safe and effective. Rigorous methodology, including double-blind studies and placebo-controlled trials, is essential for accurate conclusions. The results of clinical trials are crucial for informing treatment guidelines and recommendations.
Key Research Areas and Potential Future Directions
| Research Area | Potential Future Directions |
|---|---|
| Pharmacological Interventions | Development of targeted therapies that specifically address the underlying molecular mechanisms of MCI, such as those linked to amyloid-beta plaques and tau tangles. Trials on combination therapies to improve efficacy and reduce side effects. |
| Lifestyle Modifications | Longitudinal studies to evaluate the long-term effects of interventions such as diet, exercise, and social engagement on cognitive function and the risk of progression. Development of tailored lifestyle programs for individuals with MCI, taking into account their specific needs and preferences. |
| Diagnostic Tools | Development of more sensitive and specific diagnostic tools that can identify individuals at risk of MCI earlier and more accurately. Focus on blood biomarkers and neuroimaging techniques. |
| Personalized Medicine | Tailoring treatment approaches to individual genetic profiles, lifestyle factors, and cognitive characteristics. Using predictive modeling to identify individuals likely to benefit from specific interventions. |
Outcome Summary
In conclusion, mild cognitive impairment treatment offers a diverse range of options to help manage symptoms and improve outcomes. By combining non-pharmacological interventions, such as cognitive training and lifestyle adjustments, with potential pharmacological approaches, individuals with MCI can potentially experience significant improvements in their cognitive abilities and overall well-being. Continued research and advancements in this field promise even more effective and personalized treatment strategies in the future.
Popular Questions
What are the common symptoms of mild cognitive impairment?
Common symptoms include subtle memory problems, difficulty with language, or trouble with planning and organizing. The severity and frequency of these symptoms can vary greatly.
How is mild cognitive impairment diagnosed?
Diagnosis involves a thorough evaluation, including cognitive testing, medical history, and neurological examination.
Are there any medications to treat mild cognitive impairment?
Currently, there aren’t any medications specifically approved for treating MCI. However, some medications may be used to manage related symptoms.
What role does diet play in preventing mild cognitive impairment?
A balanced diet rich in fruits, vegetables, and omega-3 fatty acids is important for overall brain health and may help reduce the risk of MCI.

